Abstract
Vaccination is a powerful tool to reduce the burden of infectious diseases in paediatric patients with chronic rheumatic diseases. Live attenuated vaccines are not recommended for profoundly immunosuppressed patients, but nonlive vaccines have adequate safety and efficacy profiles in the few (admittedly underpowered) studies published to date. No severe vaccine-specific or disease-specific adverse events have been observed in patients with juvenile idiopathic arthritis (JIA) or childhood-onset systemic lupus erythematosus (SLE) who have been vaccinated with live or nonlive agents. The immune response to live vaccines is variable in these patients but generally adequate, despite concomitant use of immunosuppressive and biologic agents. The proposal that onset of autoimmune rheumatic diseases could be induced by vaccination is controversial and primarily based on case reports; however, patients with mevalonate kinase deficiency can experience febrile attacks after immunizations. Adequately powered studies of live and nonlive vaccination in patients with paediatric rheumatic diseases are necessary to clarify safety and efficacy issues. This narrative Review discusses vaccination in patients with JIA, childhood-onset SLE, juvenile dermatomyositis, juvenile systemic sclerosis, primary vasculitis and autoinflammatory syndromes. Vaccine safety, short-term and long-term changes in disease parameters, and the immunogenicity and influence of immunosuppressive agents are outlined for each combination of disease and vaccine.
Key Points
-
Nonlive vaccines have adequate safety profiles and are highly recommended for use in paediatric patients with rheumatic diseases
-
Live attenuated vaccines are generally not recommended for profoundly immunosuppressed patients, including those receiving high doses of ciclosporin, azathioprine, methotrexate or corticosteroids
-
Most published studies of vaccination in paediatric patients with rheumatic diseases were not adequately powered to assess immunogenicity and safety
-
No serious adverse events have been reported in patients with juvenile idiopathic arthritis or childhood-onset systemic lupus erythematosus immunized with either live or nonlive vaccines
-
The immune response to vaccination with nonlive agents in these two groups of patients was variable but generally adequate, despite concurrent use of immunosuppressive and biologic agents
-
The proposal that autoimmune rheumatic diseases could be induced after vaccination is controversial, although patients with mevalonate kinase deficiency might experience febrile attacks after immunizations
Similar content being viewed by others
Introduction
Children and adolescents with chronic rheumatic diseases, including juvenile idiopathic arthritis (JIA), childhood-onset systemic lupus erythematosus (SLE), juvenile dermatomyositis (JDM), primary vasculitis and autoinflammatory syndromes are particularly susceptible to infections, as a result of both the disease itself and immunosuppressive therapies. Vaccination is highly specific, inexpensive and safe in healthy paediatric populations and is, therefore, one of the main tools used to reduce the morbidity associated with viral and bacterial infections.1,2 Live and nonlive vaccines are included in routine paediatric vaccination programs worldwide. However, immunization of patients with childhood inflammatory conditions is somewhat controversial, particularly because of concerns over vaccine safety and effectiveness, related to the distinct disease manifestations and their respective treatments.3,4,5 Moreover, in some patients, vaccines that require administration with adjuvants have induced autoantibodies, and even overt autoimmune disease—a condition termed autoimmune/inflammatory syndrome induced by adjuvants (ASIA).3 This condition is caused by environmental factors with an immune adjuvant effect such as silicone, aluminium, pristane, and infectious components that can induce autoimmune disease. ASIA is characterized by muscular and joint manifestations, chronic fatigue, sleep disturbances, cognitive impairment and memory loss, and the possible emergence of a demyelinating autoimmune disease.3
The lack of a clear definition of vaccine immunogenicity and safety among children and adolescents with rheumatic diseases hampered the identification of indications and contraindications for vaccination, with consequently inadequate surveillance of vaccinated patients by paediatric rheumatologists.6,7,8,9 In 2011, a European League Against Rheumatism (EULAR) task force published a systematic review10 and an article in which the Delphi voting procedure was used to determine the level of agreement on 15 evidence-based recommendations1 for vaccinating patients with paediatric rheumatic diseases. Both publications reinforced the need for regular updates, as the majority of recommendations were weak. Nonlive vaccines are, however, highly recommended for patients with JIA, childhood-onset SLE, JDM or juvenile systemic sclerosis.1 By contrast, live attenuated vaccines are not recommended in profoundly immunosuppressed patients.1 According to the American Academy of Pediatrics and The Committee of Immunization Practices of the Centers for Disease Control and Prevention in the USA, profound immunosuppression was defined as current use or use in the past 3 months of any dose of mycophenolate mofetil, cyclophosphamide or methylprednisolone; ciclosporin (>3.0 mg/kg daily), azathioprine (>1.5 mg/kg daily), methotrexate (>0.4 mg/kg or 28 mg weekly) or corticosteroids (>2.0 mg/kg or >20 mg daily for more than 1 week); or combinations of these drugs with other immunosuppressive agents.11,12 The EULAR task force did not discuss a consensus opinion on the potential role of immunization in inducing or aggravating paediatric rheumatic diseases.1,10
The results of appropriately powered studies that calculated sample sizes on the basis of immunogenicity,3,13,14 and data on vaccination of patients with paediatric autoimmune rheumatic and autoinflammatory diseases,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32 suggest that a consolidated approach to vaccinating patients with these conditions is needed. This Review focuses on each disease individually, examines the short-term and long-term safety of live attenuated and nonlive composite vaccines, and discusses whether the immunogenicity of each vaccine is influenced by disease-related factors or treatment with immunosuppressive agents. However, no data exist regarding live attenuated vaccines for poliovirus or yellow fever or nonlive inactivated vaccines against poliovirus, Haemophilus influenza type b or human papilloma virus in paediatric patients with rheumatic diseases; these vaccines are, therefore, not discussed in this Review.
The developing immune system
The immune response in children, especially young children (<5 years old), is weaker than in adults.33 Indeed, infants who are born prematurely (<37 weeks gestation) or have a low birth weight (<2.5 kg) consequently have an increased risk of morbidity and mortality from vaccine-preventable diseases.34 The adaptive immune system is underdeveloped in utero owing to restricted exposure to antigens. Neonates are, therefore, largely dependent on the innate immune system to ward off disease;35 the attenuated type 1 T-helper (TH1) response alters the effectiveness of the response to vaccines in infants and increases their susceptibility to intracellular infections compared with older children.33,35 TH1 cell-mediated immunity increases rapidly from 6 months after birth and the immune system continues to mature until the child is 5 years old, when the TH1 cell-driven immune response is comparable to that of adults.33 Nonetheless, the total T-cell count in neonates, including CD4+ and CD8+ T cells, is twice that in adults. The number of CD4+ T cells increases and the CD8+ T-cell count remains stable until the age of 2 years, when both start to decline, reaching adult levels during adolescence.33 During early infancy, the B-cell response is also less than that of adults, with a delayed onset, a shorter antibody response, lower IgG2 titres and reduced immunoglobulin affinity.35 Consequently, the humoral response to vaccines administered during the first 2 months of life does not always guarantee protective antibody titres.
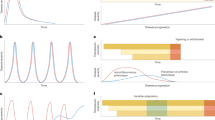
An adequate immune response to vaccines depends mainly on B-cell responses, although T cells could also have important roles.6,36 Vaccine administration induces adaptive immune responses through the activation of antigen-presenting cells (APCs) such as dendritic cells. In the lymph nodes, the antigens are presented to T cells by the APCs, resulting in the activation and the clonal expansion of CD4+ and CD8+ T cells. CD8+ T cells can differentiate into memory and effector cells, and CD4+ T cells differentiate into several T-helper cell subtypes and assist in the activation of B cells. Naive B cells differentiate into memory B cells and antibody-secreting plasma cells. Memory B and T cells provide long-term immunity in the blood, lymph nodes and the bone marrow (Figure 1).
Vaccine antigens are recognized by APCs in the lymph nodes. The antigens are then presented to T cells, inducing their activation and the clonal expansion of CD4+ and CD8+ T cells that can differentiate into effector and memory cells respectively. The CD4+ T cells can also differentiate into TH cells that assist in the activation of B cells. The naive B cells differentiate into memory B cells or antibody-secreting B cells. Memory B and T cells guarantee long-term immunity. Abbreviations: APC, antigen presenting cell; TH, T helper.
Indeed, both B-cell and T-cell defects can influence the effectiveness of immunization in patients with primary immunodeficiencies or those who are being treated with immunosuppressive therapy.13,35,36 These children usually have a reduced immune response to vaccines and could also develop active infections after immunization with live agents.37 Furthermore, if onset of paediatric rheumatic diseases (such as childhood-onset SLE and JDM)27,30 occurs during the development of the immune system, the pathogenic processes underlying these diseases could influence both the specific T-cell response to vaccination and the resulting memory B-cell population.
Juvenile idiopathic arthritis
Live vaccines
Vaccine safety
Possible adverse events related to vaccination could involve either worsening of the pre-existing rheumatic disease or reactions to the vaccination itself, including localized or systemic anti-inflammatory reactions as well as overt disease (for live attenuated vaccines). Live attenuated vaccines, including those based on measles, mumps and rubella (MMR), varicella-zoster and bacillus Calmette–Guérin (BCG), seem to be safe to use in patients with JIA (Table 1).20,38,39,40,41,42,43
The MMR vaccine is usually administered at 14–15 months of age with a booster at 8–10 years of age.20,39 A retrospective observational study was performed to evaluate the MMR vaccine booster in 207 patients with JIA.39 Disease-specific and vaccine-specific safety of this vaccine was adequate, with no evidence of increased JIA activity or vaccine-related severe adverse events (including overt measles, mumps or rubella) during the 6 months after immunization;39 similar results were also reported in a small prospective study.40 Moreover, no deterioration in erythrocyte sedimentation rate was observed after MMR vaccination in 49 patients with JIA who were being treated with methotrexate.39 However, a mild exacerbation of JIA within the 8 weeks following rubella-only vaccination was reported in 85 patients with JIA.38 To our knowledge, only one case report describes a relapse of JIA temporally associated with vaccination. Relapse occurred 5 days after administration of a live attenuated rubella-only vaccine in a patient with systemic-onset JIA who was in long-term remission.41
In a prospective, controlled study,43 25 patients with juvenile rheumatic diseases, 17 of whom had JIA, received a single dose of varicella-zoster vaccine. All patients were being treated with methotrexate and five patients with JIA were also receiving prednisone (up to 10 mg daily).43 None of the 25 patients with a juvenile rheumatic disease or the 18 healthy children in this study developed varicella after immunization.43 One patient with a juvenile rheumatic disease and one healthy child had a low-grade fever, and three patients with JIA developed a self-limited, varicella-like rash.43 No disease activity parameter worsened during the 3 months after vaccination.43 Of note, the number of active joints in the patients with JIA decreased significantly after immunization (P = 0.009).43
Immunogenicity and immunosuppressive agents
The immunogenicity of live attenuated vaccines is generally reduced in patients with JIA compared with healthy children; however, therapy does not seem to account for this deleterious effect.1 In a controlled study,40 lower antibody titres were produced in response to the measles component of the MMR vaccine in patients with JIA compared with healthy children, 6 months after immunization. The immune response to the MMR vaccine comprises both humoral and cell-mediated elements,44 but neither humoral nor cellular immune responses were substantially altered by low doses of methotrexate, alone or in combination with anti-TNF therapy, in patients with JIA who received the MMR vaccine.40 The long-term antibody response to MMR and diphtheria vaccines was evaluated in a retrospective cross-sectional study of 400 patients with JIA and 2,176 healthy children.20 Up to 5 years after vaccination, the patients with JIA had lower seroprotection rates as well as lower geometric mean titres (GMTs) of antibodies against mumps, rubella and diphtheria than those of the healthy children. By contrast, the measles-specific GMT was substantially higher in patients with JIA than healthy children, and seroprotection rates were comparable to those in healthy patients. Immunogenicity of the measles vaccine was not affected by treatment with immunosuppressive agents, particularly methotrexate or glucocorticoids.20
The humoral immune response in 17 patients with JIA of all subtypes was similar to that of controls after one dose of a live attenuated varicella-zoster vaccine.43 Eight patients with JIA maintained seroprotective levels of virus-specific IgG antibodies 1 year after immunization.43
The (tuberculin) purified protein derivative skin test was performed in 115 children with JIA who had been vaccinated with BCG.42 Immunogenicity (in terms of both induration size and test positivity rate) was significantly lower in immunized patients with JIA than in healthy, immunized children.42
Nonlive vaccines
Vaccine safety
Adequate safety profiles for vaccines against influenza, pneumococcal and meningococcal infections, hepatitis B and hepatitis A have been observed in patients with JIA (Table 2).15,22,25,26,45,46,47,48,49,50 In general, clinical and laboratory disease activity parameters remained stable after influenza immunization.14,16,45,46,47 A prospective evaluation of 34 paediatric patients with chronic arthritis found no significant increase in disease activity parameters after seasonal influenza vaccination.45 Likewise, in a study of influenza vaccination in children with rheumatic diseases (including 49 patients with JIA) who were being treated with long-term immunosuppressive therapy, no patients had disease flares 1, 3, or 6–8 months after vaccination.47 These observations, which indicate the safety of seasonal influenza vaccination, have been reinforced by the findings of a study in 31 patients with stable JIA,21 in which no safety concerns were reported 1 month or 5 months after immunization. Additionally, the safety profile of the vaccine administered with MF59 adjuvant was no worse in children and adolescents with JIA than in healthy individuals.16 The most frequent adverse events related to this vaccine were mild, local reactions.14,21,22,45
Notably, autoantibody induction by seasonal influenza vaccine was assessed in one study of 49 children and adolescents with JIA; no increase in autoantibody titre was observed.47 Likewise, rheumatoid factor levels remained stable in 60 patients with JIA who were immunized with seasonal influenza vaccine.16 By contrast, a trend towards increased levels of anticardiolipin IgG after receiving seasonal influenza vaccination was observed in a prospective study of 31 patients with JIA: such antibodies were present in 10%, 20% and 32% of patients before, 1 month after, and 6 months after immunization, respectively.21 No changes were observed in the levels of antinuclear antibodies, antineutrophil cytoplasmic antibodies, anti-β2 glycoprotein I antibodies or lupus anticoagulant.
In one case report,23 a 3-year-old patient with systemic-onset JIA relapsed after receiving two doses of influenza vaccine. However, short-term severe adverse events and disease exacerbation were not observed after influenza vaccination in 27 paediatric patients with systemic-onset JIA who were being treated with tocilizumab.24 The use of adjuvant-free pandemic influenza A H1N1/2009 vaccine also had a satisfactory disease-specific safety profile; patients with JIA had stable disease parameters before and after immunization.14
Pneumococcal infections are associated with increased morbidity and mortality in patients being treated with anti-TNF agents.49 Vaccination against pneumococcal and meningococcal infections, as well as hepatitis A and B, is safe in patients with JIA. Only mild, local reactions in response to vaccination against pneumococcal infections were reported in 31 patients with JIA who were receiving conventional DMARDs along with anti-TNF therapy and in 32 age-matched patients treated only with conventional DMARDs.49 In a multicentre study,50 234 patients with JIA aged 1–19 years received a meningococci serogroup C conjugate vaccine. Clinical and laboratory parameters of disease activity remained stable in these patients throughout the 6 months before and 6 months after vaccination.50 In the only study that has evaluated hepatitis B vaccination in patients with JIA who were in disease remission at the time of vaccination,48 none of the 39 patients (aged 4–16 years) had clinical deterioration or any other adverse event related to the vaccine. Similar findings were reported in a study of the effect of administering two doses of hepatitis A vaccine in 47 children with JIA.25
Immunogenicity and immunosuppressive agents
Antibody production induced by nonlive vaccines is variable in patients with JIA, and reduced antibody titres have been found in children with JIA after receiving nonlive vaccines.47,48,50 Antibody responses to these vaccines were generally not affected by therapy with glucocorticoids or conventional DMARDs, including methotrexate, with the exception of anti-TNF therapy, which mildly decreased the antibody response.1,16,25,49
Immunization against seasonal influenza produced adequate seroprotection rates in a short-term assessment.16,21,45 Protective antibody titres in patients with JIA were comparable to those in healthy controls 6 months after vaccination.21 The vaccine was adequately tolerated in children with JIA who were concomitantly treated with immunosuppressive drugs;16 however, this vaccine had reduced immunogenicity in patients treated with etanercept compared with healthy controls.16 The use of MF59 adjuvant vaccines resulted in comparable seroprotection and seroconversion rates to seasonal influenza A (H1N1 and H2N3 strains) in 30 patients with JIA treated with conventional DMARDs, 30 patients with JIA treated with etanercept and 30 healthy children.16 However, seroconversion and seroprotection rates, as well as GMTs to the influenza B strain, were significantly lower in individuals receiving anti-TNF therapy than in patients receiving conventional DMARDs or healthy individuals (P <0.05).16 Therapy duration did not affect these immunogenicity end points.16
No significant differences in immunogenicity after immunization against influenza were observed between patients with systemic-onset JIA treated with an anti-IL-6 agent (tocilizumab) and healthy individuals.24 Moreover, the duration of anti-IL6 therapy and the dose of glucocorticoids used did not influence the immune response in this subgroup of patients with JIA.24
Pandemic influenza vaccines are approved for use in patients with juvenile rheumatic diseases if the following three current immunologic standards proposed by the European Medicines Agency (EMA) and FDA are met: seroprotection rate >70%, seroconversion rate >40% and a GMT increase of >2.5-fold from baseline.51,52,53 In a prospective study including 95 patients with JIA and 91 healthy people, the patients with JIA had an adequate seroprotection rate (88.4%) but the seroconversion rate was lower than that in healthy controls (83.2% and 95.6%, respectively, still within the EMA and FDA criteria) after vaccination with a pandemic influenza A H1N1/2009 vaccine.14 Importantly, JIA subtype and treatment with immunosuppressive drugs, including methotrexate and anti-TNF agents, did not influence these immunogenicity parameters.
A septivalent pneumococcal conjugate vaccine generated protective titres of antibodies in 87–100% of patients with JIA who were treated with both an anti-TNF agent and DMARDs, and in 93–100% of those treated solely with conventional DMARDs.49 Nevertheless, the GMTs against serotypes 4, 14 and 23F were significantly lower in patients treated with an anti-TNF agent plus DMARDs than in those treated with DMARDs alone (P <0.05).49 All patients with systemic-onset JIA were immunized using a 23-valent pneumococcal polysaccharide vaccine in a randomized, placebo-controlled study of the IL-1 receptor antagonist anakinra.26 An adequate and persistent antibody response was mounted by immunized patients treated with anakinra, but the antibody response in patients treated with placebo was not sustained 12 months after immunization.26 The immune response to meningococci serogroup C conjugate vaccine was adequate in a prospective study,50 as seroprotective antibody titres were achieved in 153 (98%) patients with JIA, in spite of the concurrent use of immunosuppressive drugs.
In a controlled study of hepatitis B immunization,25 38 (97%) patients with JIA of all subtypes developed effective humoral responses, albeit with considerably lower GMTs than were obtained in healthy children. Patients vaccinated at 0, 1 and 6 months of age had a trend towards better responsiveness than those vaccinated at 0, 1 and 3 months of age.25 Similarly, significantly lower levels of IgG antibodies against hepatitis A virus were produced in response to immunization in patients with JIA than in healthy individuals.25 Of note, all four patients in this study who did not undergo seroconversion had active systemic-onset JIA and were being treated with anti-TNF therapy.25
Childhood-onset SLE
Live vaccines
Vaccine safety
The safety of live attenuated vaccines in patients with childhood-onset SLE has only been evaluated for varicella-zoster vaccine (Table 3).19 A prospective and controlled study was carried out in 54 patients with childhood-onset SLE who were randomly assigned to receive or not receive varicella-zoster vaccine, along with 28 healthy children (all of whom were immunized).19 No differences in adverse events or flares were observed between the vaccinated groups. During follow up, four cases of herpes zoster were reported in the nonvaccinated patients with childhood-onset SLE, whereas no cases of herpes zoster were reported in the vaccinated group.19
Immunogenicity and immunosuppressive agents
Data on the immunogenicity of live attenuated vaccines in patients with childhood-onset SLE are scarce (Table 3). In the varicella-zoster vaccination study described above,19 the production of IFN-γ by T cells stimulated ex vivo with varicella-zoster virus antigen was lower in immunized patients with childhood-onset SLE than in the immunized healthy individuals, who were not taking immunosuppressive drugs. IFN-γ could be involved in the pathogenesis of SLE and could also interfere with the response to vaccination with varicella-zoster virus antigen.
A 2011 study evaluated the immunogenicity of a measles vaccine in 18 patients with childhood-onset SLE and 11 people who completed all their childhood vaccinations before the onset of SLE.18 The levels of measles antibodies were similar between these groups.18
Nonlive vaccines
Vaccine safety
Influenza, hepatitis B and tetanus vaccines are safe to use in patients with childhood-onset SLE (Table 3).15,18,27,28,29,47,54 Seasonal influenza vaccine was well tolerated, and no severe adverse effects were documented in a few studies with small samples of patients with childhood-onset SLE.15,47 An adjuvant-free pandemic influenza A H1N1/2009 vaccine was examined in a prospective study including 118 patients with childhood-onset SLE and 102 healthy children of comparable age.27 No change in the median SLE Disease Activity Index (SLEDAI)-2000 score was found 21 days or 4 months after immunization compared to preimmunization scores.27 The frequencies of articular, neuropsychiatric and haematological abnormalities in these patients also remained stable, although a significant decrease in renal involvement and a significant increase in mucocutaneous lesions were observed 4 months after vaccination (P <0.05).27 No serious adverse events attributable to the vaccine were reported.27 These patients had stable autoantibody profiles (no change in the levels or specificities of autoantibodies) before and after vaccination;27 similar results were also observed in 11 patients with childhood-onset SLE who were immunized against seasonal influenza.47
Only one study has assessed hepatitis B vaccination in patients with childhood-onset SLE.28 In this study,28 20 patients with SLEDAI scores <10 and 24 healthy people were vaccinated with three doses of a recombinant hepatitis B vaccine at 0, 1 and 6 months. Disease flare frequency was comparable to that in a nonvaccinated group of patients with childhood-onset SLE (15% versus 18%, respectively), and the mean SLEDAI score was constant after the vaccination scheme was completed.28 No adverse events related to the vaccine were observed.28
Immunogenicity and immunosuppressive agents
Antibody production induced by nonlive vaccines is variable in patients with childhood-onset SLE. Adequate seroconversion rates were observed in patients who received hepatitis B and tetanus vaccines.28,54 Immunosuppressive therapy had no effect on the immunogenicity of influenza vaccines, however humoral and cell-mediated immune responses to both pandemic influenza A H1N1 vaccine and trivalent seasonal influenza vaccine were lower in high-risk immunosuppressed children and adolescents than in healthy individuals.29 The high-risk group included 20 patients with childhood-onset SLE, 80% of whom were treated with prednisone and 35% with mycophenolate mofetil.29 The pandemic influenza vaccine achieved seroprotection in only 45% of patients with childhood-onset SLE;29 moreover, although 60% of patients with childhood-onset SLE responded to the seasonal vaccine initially, these individuals had a more rapid decline in antibody titres than occurred in healthy children or patients with asthma.29 Of note, patients with childhood-onset SLE had a lower cell-mediated response to the H1N1/2009 pandemic influenza vaccine than patients with asthma, sickle cell disease, or recipients of solid-organ graft, as measured by enzyme-linked immunosorbent spot assay.29
Likewise, immunogenicity parameters were also generally reduced in patients with childhood-onset SLE relative to their levels in healthy individuals after receiving the pandemic influenza vaccine.27 The main factors associated with a lack of seroconversion were a SLEDAI-2000 score ≥8 and a high mean current glucocorticoid dose.27 After multivariate logistic regression analysis, high SLEDAI-2000 score was the most important variable associated with the lack of seroconversion.27
By contrast, the immunogenicity of a hepatitis B vaccine was adequate in a prospective controlled study of a small population of patients with childhood-onset SLE.28 Seroconversion rates were similar in patients with childhood-onset SLE and healthy individuals 1 month after the third vaccine dose (80% and 100%, respectively), despite reduced GMTs in the patients with childhood-onset SLE.28 Vaccine immunogenicity was not influenced by immunosuppressive treatment.28
The humoral response to tetanus vaccine was evaluated in a controlled study including 40 patients with childhood-onset SLE and 60 healthy people matched for age and sex.54 Protective titres of antitetanus antibody were produced in both patients and controls, and GMTs were also similar in both groups, despite the use of glucocorticoids and other immunosuppressive drugs in 90% of the patients with childhood-onset SLE.54 Reinforcing this finding, in another study that evaluated the immunogenicity of tetanus vaccine,18 patients who had received all their childhood vaccinations before onset of SLE had a comparable seroprotection rate to that in patients with childhood-onset SLE and healthy people.
Juvenile dermatomyositis
The hypothesis that immunization can induce JDM is controversial. The temporal relationship between vaccinations against hepatitis B, diphtheria, pertussis, tetanus, poliomyelitis, smallpox and tuberculosis and the onset of JDM symptoms is restricted to a few case reports, and no causal relationship has been proven (Table 4).55,56,57,58
Data regarding the safety of live attenuated vaccines in patients with JDM are scarce. In the only report to date,43 no worsening of disease activity and no serious vaccine-related adverse effects occurred in four patients with JDM who received a live attenuated vaccine against varicella-zoster. Two of these patients produced protective levels of antibodies.43 All four patients were taking prednisone (up to 10 mg daily) and methotrexate.43
Vaccine-induced antibody production was reduced in patients with JDM who received a nonlive vaccine against pandemic influenza, although vaccine-specific and disease-specific safety were both adequate.15,30 The largest study to evaluate vaccination using nonlive agents in patients with JDM was a prospective, open-label, controlled study that included 30 patients with JDM and 81 healthy children and adolescents who were vaccinated against the pandemic influenza A strain H1N1/2009.30 No clinical or laboratory findings suggestive of increased disease activity were reported 3 weeks after vaccination, and only mild adverse events were observed.30 After immunization, seroconversion rates were markedly lower in patients with JDM than in healthy individuals, despite similar seroprotection rates, GMTs and increases in GMTs in both groups.30 Lack of seroconversion was associated with a chronic disease course, prednisone doses >20mg daily and use of a combination of prednisone, methotrexate and ciclosporin.30 Another study including six patients with JDM immunized with a nonlive vaccine against seasonal influenza also reported no vaccine-related severe adverse events or disease flares.15
Juvenile systemic sclerosis
Rare case reports suggest a temporal relationship between hepatitis B, diphtheria, pertussis, tetanus and MMR vaccinations and the onset of juvenile systemic sclerosis, particularly deep morphea.59,60,61 Whether these associations represent a causal relationship is not currently known. However, no worsening of disease parameters and no serious adverse events were reported in three patients with juvenile systemic sclerosis who received live attenuated varicella-zoster vaccine (Table 4).43 Protective antibody levels were reached in two of the three patients, all of whom were taking prednisone (up to 20 mg daily) and methotrexate.43
Furthermore, in 237 patients with juvenile rheumatic diseases, only the 11 patients with juvenile systemic sclerosis produced titres of vaccine-induced antibodies that were comparable to those of healthy patients in response to vaccination (using a nonlive agent) against pandemic influenza.13 A reduced immune response was observed in patients with JIA, childhood-onset SLE, JDM or primary vasculitis.13 No severe adverse events related to vaccination were observed in any patient in this study.13
Juvenile primary vasculitis
Several reports describe the onset of primary vasculitis, especially Henoch–Schönlein purpura (HSP)31,62,63,64,65,66,67 and Kawasaki disease,68,69 after administration of either live or nonlive vaccines. However, no increase in the incidence or recurrence of HSP was observed within 30 days after administration of a nonlive vaccine against group B meningococci in a New-Zealand-wide immunization campaign involving children aged 6 weeks to 10 years.70 Similarly, in a retrospective analysis of data from a vaccine safety database, no new cases of HSP were found within the 42 days after administration of a total of 49,027 doses of meningococcal polysaccharide vaccine to a population of adolescents and young adults 16–20 years old.62 Additionally, two retrospective studies found no association between the onset of Kawasaki disease and vaccinations, including with septivalent pneumococcal conjugate vaccine71 and live rotavirus oral vaccine.72
Induration and inflammation at a previous BCG immunization site has aided in the diagnosis of complete and incomplete Kawasaki disease.73,74,75,76,77,78 Indeed, in a nationwide Japanese epidemiological survey, redness or crust formation at a prior BCG inoculation site was observed in 50% of the 15,524 patients with Kawasaki disease who had a history of BCG vaccination.79
The immunogenicity and safety of an adjuvant-free, nonlive influenza A H1N1/2009 vaccine has been studied in patients with juvenile autoimmune rheumatic diseases (Table 4).13 The participants included 16 patients with a primary vasculitis: HSP (n = 5), Takayasu arteritis (n = 3), granulomatosis with polyangiitis (n = 3), polyarteritis nodosa (n = 3), Kawasaki disease (n = 1) and Behçet disease (n = 1).13 Seroconversion rates were considerably lower in the patients with primary vasculitis than in healthy individuals, 3 weeks after vaccination, despite comparable seroprotection rates, GMTs and factor increases in GMT.13 No severe vaccine-related adverse events were reported.13 In another study of five paediatric patients with primary vasculitis, a disease flare occurred in one patient with Takayasu arteritis within 2 weeks of receiving a nonlive vaccine against seasonal influenza.15 The flare stabilized after the patient's dosage of prednisolone was increased.
Autoinflammatory syndromes
Patients with mevalonate kinase deficiency (hyper IgD syndrome) might experience an inflammatory episode, especially a febrile attack, after receiving childhood immunizations (Table 4).80 In a prospective observational study of 11 patients with mevalonate kinase deficiency,32 anakinra treatment prevented the attacks of fever associated with diphtheria, tetanus and pertussis vaccination in three of these patients, without inhibiting antibody induction.
Conclusions
The majority of studies of vaccination in paediatric patients with rheumatic diseases have been performed in small populations and were, therefore, insufficiently powered to determine the immunogenicity and safety of the vaccine. Most such studies were performed using nonlive vaccines in patients with JIA or childhood SLE, among whom no severe adverse events relating to either the vaccine or the underlying disease were reported. The vaccine-induced immune response was variable but generally adequate, despite the concurrent use of immunosuppressive and biologic agents. Studies of live vaccines in paediatric patients with rheumatic diseases are scarce, but no serious adverse events have been reported in patients with either JIA or childhood-onset SLE.
The suggestion that onset of autoimmune rheumatic diseases might be triggered by vaccination is controversial, and no causal relationship has yet been demonstrated. Patients with mevalonate kinase deficiency could, however, experience febrile attacks after immunizations. Adequately powered studies of the immune response to live and nonlive vaccines, and further evaluation of disease-specific and vaccine-specific safety profiles and the influence of immunosuppressive therapy are necessary in populations of patients with all paediatric rheumatic diseases.
Review criteria
We searched for original articles focusing on immunization in patients with paediatric rheumatic diseases in MEDLINE and PubMed, published between 1970 and 2012. The search terms we used, in various combinations, were “vaccine”, “immunization”, “paediatric rheumatic diseases”, “children”, “juvenile idiopathic arthritis”, “juvenile rheumatoid arthritis”, “juvenile systemic lupus erythematosus”, “childhood-onset systemic lupus erythematosus”, “juvenile dermatomyositis”, “scleroderma”, “vasculitis”, “Henoch–Schönlein purpura”, “Kawasaki syndrome”, “polyarteritis nodosa”, “granulomatous polyangiitis”, “Wegener granulomatosis”, “Behçet disease”, “Takayasu arteritis”, “autoinflammatory syndromes”, “immunogenicity” and “safety”. All articles identified were English-language full-text papers. We also searched the reference lists of identified articles for further papers.
References
Heijstek, M. W. et al. EULAR recommendations for vaccination in paediatric patients with rheumatic diseases. Ann. Rheum. Dis. 70, 1704–1712 (2011).
Janow, G. & Ilowite, N. T. Pediatric rheumatic disease: vaccination in pediatric rheumatic disease—risks and benefits. Nat. Rev. Rheumatol. 8, 188–190 (2012).
Shoenfeld, Y. & Agmon-Levin, N. 'ASIA'—autoimmune/inflammatory syndrome induced by adjuvants. J. Autoimmun. 36, 4–8 (2011).
Dell'Era, L., Esposito, S., Corona, F. & Principi, N. Vaccination of children and adolescents with rheumatic diseases. Rheumatology (Oxford) 50, 1358–1365 (2011).
Frenck, R. W. & Seward, J. F. Varicella vaccine safety and immunogenicity in patients with juvenile rheumatic diseases receiving methotrexate and corticosteroids. Arthritis Care Res. (Hoboken) 62, 903–906 (2010).
Silva, C. A. et al. Vaccination practice in children with rheumatic disease. Rev. Bras. Reumatol. 50, 351–361 (2010).
Davies, K. & Woo, P. British Paediatric Rheumatology Group. Immunization in rheumatic diseases of childhood: an audit of the clinical practice of British Paediatric Rheumatology Group members and a review of the evidence. Rheumatology (Oxford) 41, 937–941 (2002).
Morin, M. P., Quach, C., Fortin, E. & Chédeville G. Vaccination coverage in children with juvenile idiopathic arthritis followed at a paediatric tertiary care centre. Rheumatology (Oxford) 51, 2046–2050 (2012).
McCann, L. J. Should children under treatment for juvenile idiopathic arthritis receive flu vaccination? Arch. Dis. Child. 92, 366–368 (2007).
Heijstek, M. W. et al. Vaccination in paediatric patients with auto-immune rheumatic diseases: a systemic literature review for the European League against Rheumatism evidence-based recommendations. Autoimmun. Rev. 11, 112–122 (2011).
American Academy of Pediatrics. Red Book: 2003 Report of the Committee of Infectious Diseases 26th edn 672–686 (American Academy of Pediatrics, 2003).
Cush, J. J. & Kavanaugh, A. Herpes zoster (shingles) vaccine guidelines for immunosuppressed patients. American College of Rheumatology: Hotline [online] (2008).
Aikawa, N. E. et al. Corticosteroid: major factor for reduced immunogenicity of 2009 influenza A (H1N1) vaccine in patients with juvenile autoimmune rheumatic disease. J. Rheumatol. 39, 167–173 (2012).
Aikawa N. et al. Effective seroconversion and safety following the pandemic influenza vaccination (anti-H1N1) in patients with juvenile idiopathic arthritis. Scand. J. Rheumatol. 42, 34–40 (2013).
Ogimi, C., Tanaka, R., Saitoh, A. & Oh-Ishi, T. Immunogenicity of influenza vaccine in children with pediatric rheumatic diseases receiving immunosuppressive agents. Pediatr. Infect. Dis. J. 30, 208–211 (2011).
Dell'Era, L. et al. Immunogenicity, safety and tolerability of MF59-adjuvanted seasonal influenza vaccine in children with juvenile idiopathic arthritis. Vaccine 30, 936–940 (2012).
Ronaghy, A. et al. Vaccination leads to an aberrant FOXP3 T-cell response in non-remitting juvenile idiopathic arthritis. Ann. Rheum. Dis. 70, 2037–2043 (2011).
Miyamoto, M. et al. Vaccine antibodies and T- and B-cell interaction in juvenile systemic lupus erythematosus. Lupus 20, 736–744 (2011).
Barbosa, C. M. et al. Immune response and tolerability of varicella vaccine in children and adolescents with systemic lupus erythematosus previously exposed to varicella-zoster virus. Clin. Exp. Rheumatol. 30, 791–798 (2012).
Heijstek, M. W., van Gageldonk, P. G., Berbers, G. A. & Wulffraat, N. M. Differences in persistence of measles, mumps, rubella, diphtheria and tetanus antibodies between children with rheumatic disease and healthy controls: a retrospective cross-sectional study. Ann. Rheum. Dis. 71, 948–954 (2012).
Toplak, N. et al. Safety and efficacy of influenza vaccination in a prospective longitudinal study of 31 children with juvenile idiopathic arthritis. Clin. Exp. Rheumatol. 30, 436–444 (2012).
Miraglia, J. L. et al. Immunogenicity and reactogenicity of 2009 influenza A (H1N1) inactivated monovalent non-adjuvanted vaccine in elderly and immunocompromised patients. PLoS ONE 6, 27214 (2011).
Shimizu, M., Ueno, K. & Yachie, A. Relapse of systemic juvenile idiopathic arthritis after influenza vaccination in a patient receiving tocilizumab. Clin. Vaccine Immunol. 19, 1700–1702 (2012).
Shinoki, T. et al. Safety and response to influenza vaccine in patients with systemic-onset juvenile idiopathic arthritis receiving tocilizumab. Mod. Rheumatol. 22, 871–876 (2012).
Erguven, M., Kaya, B., Hamzah, O. Y. & Tufan, F. Evaluation of immune response to hepatitis A vaccination and vaccine safety in juvenile idiopathic arthritis. J. Chin. Med. Assoc. 74, 205–208 (2011).
Quartier, P. et al. A multicentre, randomised, double-blind, placebo-controlled trial with the interleukin-1 receptor antagonist anakinra in patients with systemic-onset juvenile idiopathic arthritis (ANAJIS trial). Ann. Rheum. Dis. 70, 747–754 (2011).
Campos, L. M. et al. High disease activity: an independent factor for reduced immunogenicity of pandemic influenza a vaccine in patients with juvenile SLE. Arthritis Care Res. (in press).
Aytac, M. B. et al. Hepatitis B vaccination in juvenile systemic lupus erythematosus. Clin. Exp. Rheumatol. 29, 882–886 (2011).
Long, C. B. et al. Humoral and cell-mediated immune responses to monovalent 2009 influenza A/H1N1 and seasonal trivalent influenza vaccines in high-risk children. J. Pediatr. 160, 74–81 (2012).
Guissa, V. R. et al. Influenza A H1N1/2009 vaccine in juvenile dermatomyositis: reduced immunogenicity in patients under immunosuppressive therapy. Clin. Exp. Rheumatol. 30, 583–588 (2012).
Watanabe, T. Henoch–Schönlein purpura following influenza vaccinations during the pandemic of influenza A (H1N1). Pediatr. Nephrol. 26, 795–798 (2011).
Bodar, E. J. et al. On-demand anakinra treatment is effective in mevalonate kinase deficiency. Ann. Rheum. Dis. 70, 2155–2158 (2011).
Bodewes, R., Fraaij, P. L., Osterhaus, A. D. & Rimmelzwaan, G. F. Pediatric influenza vaccination: understanding the T-cell response. Expert Rev. Vaccines 11, 963–971 (2012).
Miller, M. A. & Rathore, M. H. Immunization in special populations. Adv. Pediatr. 59, 95–136 (2012).
PrabhuDas, M. et al. Challenges in infant immunity: implications for responses to infection and vaccines. Nat. Immunol. 12, 189–194 (2011).
Carneiro-Sampaio, M. & Coutinho, A. Tolerance and autoimmunity: lessons at the bedside of primary immunodeficiencies. Adv. Immunol. 95, 51–82 (2007).
Griffith, L. M. et al. Improving cellular therapy for primary immune deficiency diseases: recognition, diagnosis, and management. J. Allergy Clin. Immunol. 124, 1152–1160 (2009).
Linnemann, C. C., Levinson, J. E., Buncher, C. R. & Schiff, G. M. Rubella antibody levels in juvenile rheumatoid arthritis. Ann. Rheum. Dis. 34, 354–358 (1975).
Heijstek, M. W. et al. Safety of measles, mumps and rubella vaccination in juvenile idiopathic arthritis. Ann. Rheum. Dis. 66, 1384–1387 (2007).
Borte, S., Liebert, U. G., Borte, M. & Sack, U. Efficacy of measles, mumps and rubella revaccination in children with juvenile idiopathic arthritis treated with methotrexate and etanercept. Rheumatology (Oxford) 48, 144–148 (2009).
Korematsu, S. et al. A relapse of systemic type juvenile idiopathic arthritis after a rubella vaccination in a patient during a long-term remission period. Vaccine 27, 5041–5042 (2009).
Kiray, E. et al. Purified protein derivative response in juvenile idiopathic arthritis. J. Rheumatol. 36, 2029–2032 (2009).
Pileggi, G. S., de Souza, C. B. & Ferriani, V. P. Safety and immunogenicity of varicella vaccine in patients with juvenile rheumatic diseases receiving methotrexate and corticosteroids. Arthritis Care Res. (Hoboken) 62, 1034–1039 (2010).
Dhiman, N. et al. Correlations among measles virus-specific antibody, lymphoproliferation and TH1/TH2 cytokine responses following measles-mumps-rubella-II (MMR-II) vaccination. Clin. Exp. Immunol. 142, 498–504 (2005).
Malleson, P. N., Tekano, J. L., Scheifele, D. W. & Weber, J. M. Influenza immunization in children with chronic arthritis: a prospective study. J. Rheumatol. 20, 1769–1773 (1993).
Olson, N. Y. & Lindsley, C. B. Influenza immunization in children with chronic arthritis. J. Rheumatol. 21, 1581–1582 (1994).
Kanakoudi-Tsakalidou, F., Trachana, M., Pratsidou-Gertsi, P., Tsitsami, E. & Kyriazopoulou-Dalaina, V. Influenza vaccination in children with chronic rheumatic diseases and long-term immunosuppressive therapy. Clin. Exp. Rheumatol. 19, 589–594 (2001).
Kasapçopur, O. et al. Hepatitis B vaccination in children with juvenile idiopathic arthritis. Ann. Rheum. Dis. 63, 1128–1130 (2004).
Farmaki, E. et al. The effect of anti-TNF treatment on the immunogenicity and safety of the 7-valent conjugate pneumococcal vaccine in children with juvenile idiopathic arthritis. Vaccine 28, 5109–5113 (2010).
Zonneveld-Huijssoon, E. et al. Safety and efficacy of meningococcal C vaccination in juvenile idiopathic arthritis. Arthritis Rheum. 56, 639–646 (2007).
EMA. European Committee for Proprietary Medicinal Products. Guideline on dossier structure and content for pandemic influenza vaccine marketing authorisation application [online], (2004).
EMA. Committee for Proprietary Medicinal Products. Note for guidance on harmonisation of requirements for influenza vaccines [online], (1997).
US Department of Health and Human Services, Food and Drug Administration, Center for Biologics Evaluation and Research. Guidance for industry: clinical data needed to support the licensure of pandemic influenza vaccines [online], (2007).
Kashef, S., Ghazizadeh, F., Derakhshan, A., Farjadian, S. & Alyasin, S. Antigen-specific antibody response in juvenile-onset SLE patients following routine immunization with tetanus toxoid. Iran. J. Immunol. 5, 181–184 (2008).
Ehrengut, W. Dermatomyositis and vaccination. Lancet 1, 1040–1041 (1978).
Kåss, E., Straume, S., Mellbye, O. J., Munthe, E. & Solheim, B. G. Dermatomyositis associated with BCG vaccination. Scand. J. Rheumatol. 8, 187–191 (1979).
Cotterill, J. A. & Shapiro, H. Dermatomyositis after immunisation. Lancet 2, 1158–1159 (1978).
Altman, A., Szyper-Kravitz, M. & Shoenfeld, Y. HBV vaccine and dermatomyositis: is there an association? Rheumatol. Int. 28, 609–612 (2008).
Khaled, A. et al. Postvaccination morphea profunda in a child. Pediatr. Dermatol. 29, 525–527 (2012).
Benmously Mlika, R. et al. Morphea profunda in a young infant after hepatitis B vaccination. J. Am. Acad. Dermatol. 63, 1111–1112 (2010).
Torrelo, A. et al. Deep morphea after vaccination in two young children. Pediatr. Dermatol. 23, 484–7 (2006).
Goodman, M. J., Nordin, J. D., Belongia, E. A., Mullooly, J. P. & Baggs, J. Henoch–Schölein purpura and polysaccharide meningococcal vaccine. Pediatrics 126, 325–329 (2010).
Watanabe, T. & Onda, H. Henoch–Schönlein purpura with antiphospholipid antibodies following an influenza vaccination. Pediatr. Nephrol. 16, 458–459 (2001).
Ozaki, T., Miwata, H., Kodama, H., Matsui, Y. & Asano, Y. Henoch–Schönlein purpura after measles immunization. Acta. Paediatr. Jpn. 31, 484–486 (1989).
Lambert, E. M., Liebling, A., Glusac, E. & Antaya, R. J. Henoch–Schönlein purpura following a meningococcal vaccine. Pediatrics 112, e491 (2003).
Courtney, P. A., Patterson, R. N. & Lee, R. J. Henoch–Schönlein purpura following meningitis C vaccination. Rheumatology (Oxford) 40, 345–346 (2001).
Mormile, R., D'Alterio, V., Treccagnoli, G. & Sorrentino, P. Henoch–Schönlein purpura with antiphospholipid antibodies after influenza vaccination: how fearful is it in children? Vaccine 23, 567–568 (2004).
Schmöeller, D., Keiserman, M. W., Staub, H. L., Velho, F. P. & de Fátima Grohe, M. Yellow fever vaccination and Kawasaki disease. Pediatr. Infect. Dis. J. 28, 1037–1038 (2009).
Miron, D., Fink, D. & Hashkes, P. J. Kawasaki disease in an infant following immunisation with hepatitis B vaccine. Clin. Rheumatol. 22, 461–463 (2003).
Sexton, K. et al. Henoch–Schönlein purpura and meningococcal B vaccination. Arch. Dis. Child. 94, 224–226 (2009).
Center, K. J., Hansen, J. R., Lewis, E., Fireman, B. H. & Hilton B. Lack of association of Kawasaki disease after immunization in a cohort of infants followed for multiple autoimmune diagnoses in a large, phase-4 observational database safety study of 7-valent pneumococcal conjugate vaccine: lack of association between Kawasaki disease and seven-valent pneumococcal conjugate vaccine. Pediatr. Infect. Dis. J. 28, 438–440 (2009).
Hua, W. et al. Kawasaki disease after vaccination: reports to the vaccine adverse event reporting system 1990–2007. Pediatr. Infect. Dis. J. 28, 943–947 (2009).
Chalmers, D., Corban, J. G. & Moore, P. P. BCG site inflammation: a useful diagnostic sign in incomplete Kawasaki disease. J. Paediatr. Child Health 44, 525–526 (2008).
Kuniyuki, S. & Asada, M. An ulcerated lesion at the BCG vaccination site during the course of Kawasaki disease. J. Am. Acad. Dermatol. 37, 303–304 (1997).
Weinstein, M. Inflammation at a previous inoculation site: an unusual presentation of Kawasaki disease. CMAJ 174, 459–460 (2006).
Antony, D. & Jessy, P. L. Involvement of BCG scar in Kawasaki disease. Indian Pediatr. 42, 83–84 (2005).
Hsu, Y. H., Wang, Y. H., Hsu, W. Y. & Lee, Y. P. Kawasaki disease characterized by erythema and induration at the Bacillus Calmette–Guérin and purified protein derivative inoculation sites. Pediatr. Infect. Dis. J. 6, 576–578 (1987).
Sinha, R. & Balakumar, T. BCG reactivation: a useful diagnostic tool even for incomplete Kawasaki disease. Arch. Dis. Child. 90, 891 (2005).
Uehara, R., Igarashi, H., Yashiro, M., Nakamura, Y. & Yanagawa, H. Kawasaki disease patients with redness or crust formation at the Bacille Calmette–Guérin inoculation site. Pediatr. Infect. Dis. J. 29, 430–433 (2010).
Bodar, E. J., van der Hilst, J. C., Drenth, J. P., van der Meer, J. W. & Simon, A. Effect of etanercept and anakinra on inflammatory attacks in the hyper-IgD syndrome: introducing a vaccination provocation model. Neth. J. Med. 63, 260–264 (2005).
Acknowledgements
This study was sponsored by grants from the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP2008/58238-4 and FAPESP2011/12471-2 to C. A. Silva, FAPESP2009/51897-5 and FAPESP2010/10749-0 to E. Bonfa), the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq302724/2011-7 and CNPq472155/2012-1 to C. A. Silva and CNPq301411/2009-3 to E. Bonfa), the Federico Foundation (to C. A. Silva and E. Bonfa) and by Núcleo de Apoio à Pesquisa “Saúde da Criança e do Adolescente” da USP to C. A. Silva.
Author information
Authors and Affiliations
Contributions
All authors researched data for the article, discussed its content, wrote, reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Silva, C., Aikawa, N. & Bonfa, E. Vaccinations in juvenile chronic inflammatory diseases: an update. Nat Rev Rheumatol 9, 532–543 (2013). https://doi.org/10.1038/nrrheum.2013.95
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrrheum.2013.95
This article is cited by
-
Safety and immunogenicity of influenza A(H3N2) component vaccine in juvenile systemic lupus erythematosus
Advances in Rheumatology (2023)
-
Hepatitis B vaccination response of treatment-naive patients with juvenile idiopathic arthritis
Rheumatology International (2022)
-
An Update on the Management of Childhood-Onset Systemic Lupus Erythematosus
Pediatric Drugs (2021)
-
Safety and immunogenicity of the quadrivalent human papillomavirus vaccine in patients with juvenile dermatomyositis: a real-world multicentre study
Pediatric Rheumatology (2020)
-
HPV infection and vaccination in Systemic Lupus Erythematosus patients: what we really should know
Pediatric Rheumatology (2016)