Abstract
Post-translational modification and functional impairment of proteins through carbamylation is thought to promote vascular dysfunction during end-stage renal disease. Cyanate, a reactive species in equilibrium with urea, carbamylates protein lysine residues to form ε-carbamyllysine (homocitrulline), altering protein structure and function. We now report the discovery of an alternative and quantitatively dominant mechanism for cyanate formation and protein carbamylation at sites of inflammation and atherosclerotic plaque: myeloperoxidase-catalyzed oxidation of thiocyanate, an anion abundant in blood whose levels are elevated in smokers. We also show that myeloperoxidase-catalyzed lipoprotein carbamylation facilitates multiple pro-atherosclerotic activities, including conversion of low-density lipoprotein into a ligand for macrophage scavenger receptor A1 recognition, cholesterol accumulation and foam-cell formation. In two separate clinical studies (combined n = 1,000 subjects), plasma levels of protein-bound homocitrulline independently predicted increased risk of coronary artery disease, future myocardial infarction, stroke and death. We propose that protein carbamylation is a mechanism linking inflammation, smoking, uremia and coronary artery disease pathogenesis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Erill, S., Calvo, R. & Carlos, R. Plasma protein carbamylation and decreased acidic drug protein binding in uremia. Clin. Pharmacol. Ther. 27, 612–618 (1980).
Fluckiger, R., Harmon, W., Meier, W., Loo, S. & Gabbay, K.H. Hemoglobin carbamylation in uremia. N. Engl. J. Med. 304, 823–827 (1981).
Hörkkö, S., Huttunen, K., Kervinen, K. & Kesaniemi, Y.A. Decreased clearance of uraemic and mildly carbamylated low-density lipoprotein. Eur. J. Clin. Invest. 24, 105–113 (1994).
Kraus, L.M. & Kraus, A.P., Jr. Carbamoylation of amino acids and proteins in uremia. Kidney Int. Suppl. 78, S102–S107 (2001).
Stark, G.R., Stein, W.H. & Moore, S. Reactions of the cyanante present in aqueous urea with amino acids and proteins. J. Biol. Chem. 235, 3177–3181 (1960).
Bobb, D. & Hofstee, B.H. Gel isoelectric focusing for following the successive carbamylations of amino groups in chymotrypsinogen A. Anal. Biochem. 40, 209–217 (1971).
Stark, G.R. Reactions of cyanate with functional groups of proteins. II. Formation, decomposition, and properties of N-carbamylimidazole. Biochemistry 4, 588–595 (1965).
Stim, J. et al. Factors determining hemoglobin carbamylation in renal failure. Kidney Int. 48, 1605–1610 (1995).
Lhotta, K., Schlogl, A., Uring-Lambert, B., Kronenberg, F. & Konig, P. Complement C4 phenotypes in patients with end-stage renal disease. Nephron 72, 442–446 (1996).
Mun, K.C. & Golper, T.A. Impaired biological activity of erythropoietin by cyanate carbamylation. Blood Purif. 18, 13–17 (2000).
Ok, E., Basnakian, A.G., Apostolov, E.O., Barri, Y.M. & Shah, S.V. Carbamylated low-density lipoprotein induces death of endothelial cells: a link to atherosclerosis in patients with kidney disease. Kidney Int. 68, 173–178 (2005).
Nicholls, S.J. & Hazen, S.L. Myeloperoxidase and cardiovascular disease. Arterioscler. Thromb. Vasc. Biol. 25, 1102–1111 (2005).
Hazen, S.L. & Heinecke, J.W. 3-Chlorotyrosine, a specific marker of myeloperoxidase-catalyzed oxidation, is markedly elevated in low density lipoprotein isolated from human atherosclerotic intima. J. Clin. Invest. 99, 2075–2081 (1997).
Podrez, E.A., Schmitt, D., Hoff, H.F. & Hazen, S.L. Myeloperoxidase-generated reactive nitrogen species convert LDL into an atherogenic form in vitro. J. Clin. Invest. 103, 1547–1560 (1999).
Zhang, R. et al. Association between myeloperoxidase levels and risk of coronary artery disease. J. Am. Med. Assoc. 286, 2136–2142 (2001).
Brennan, M.L. et al. Prognostic value of myeloperoxidase in patients with chest pain. N. Engl. J. Med. 349, 1595–1604 (2003).
Asselbergs, F.W., Reynolds, W.F., Cohen-Tervaert, J.W., Jessurun, G.A. & Tio, R.A. Myeloperoxidase polymorphism related to cardiovascular events in coronary artery disease. Am. J. Med. 116, 429–430 (2004).
McMillen, T.S., Heinecke, J.W. & LeBoeuf, R.C. Expression of human myeloperoxidase by macrophages promotes atherosclerosis in mice. Circulation 111, 2798–2804 (2005).
Castellani, L.W., Chang, J.J., Wang, X., Lusis, A.J. & Reynolds, W.F. Transgenic mice express human MPO -463G/A alleles at atherosclerotic lesions, developing hyperlipidemia and obesity in -463G males. J. Lipid Res. 47, 1366–1377 (2006).
Abu-Soud, H.M. & Hazen, S.L. Nitric oxide is a physiological substrate for mammalian peroxidases. J. Biol. Chem. 275, 37524–37532 (2000).
Eiserich, J.P. et al. Myeloperoxidase, a leukocyte-derived vascular NO oxidase. Science 296, 2391–2394 (2002).
Baldus, S. et al. Myeloperoxidase enhances nitric oxide catabolism during myocardial ischemia and reperfusion. Free Radic. Biol. Med. 37, 902–911 (2004).
Vita, J.A. et al. Serum myeloperoxidase levels independently predict endothelial dysfunction in humans. Circulation 110, 1134–1139 (2004).
Zheng, L. et al. Apolipoprotein A-I is a selective target for myeloperoxidase-catalyzed oxidation and functional impairment in subjects with cardiovascular disease. J. Clin. Invest. 114, 529–541 (2004).
Shao, B. et al. Tyrosine 192 in apolipoprotein A-I is the major site of nitration and chlorination by myeloperoxidase, but only chlorination markedly impairs ABCA1-dependent cholesterol transport. J. Biol. Chem. 280, 5983–5993 (2005).
Zheng, L. et al. Localization of nitration and chlorination sites on apolipoprotein A-I catalyzed by myeloperoxidase in human atheroma and associated oxidative impairment in ABCA1-dependent cholesterol efflux from macrophages. J. Biol. Chem. 280, 38–47 (2005).
Wu, Z. et al. The refined structure of nascent HDL reveals a key functional domain for particle maturation and dysfunction. Nat. Struct. Mol. Biol. 14, 861–868 (2007).
Wever, R., Kast, W.M., Kasinoedin, J.H. & Boelens, R. The peroxidation of thiocyanate catalysed by myeloperoxidase and lactoperoxidase. Biochim. Biophys. Acta 709, 212–219 (1982).
Olea, F. & Parras, P. Determination of serum levels of dietary thiocyanate. J. Anal. Toxicol. 16, 258–260 (1992).
Husgafvel-Pursiainen, K., Sorsa, M., Engstrom, K. & Einisto, P. Passive smoking at work: biochemical and biological measures of exposure to environmental tobacco smoke. Int. Arch. Occup. Environ. Health 59, 337–345 (1987).
van Dalen, C.J., Whitehouse, M.W., Winterbourn, C.C. & Kettle, A.J. Thiocyanate and chloride as competing substrates for myeloperoxidase. Biochem. J. 327, 487–492 (1997).
Kersten, H.W., Moorer, W.R. & Wever, R. Thiocyanate as a cofactor in myeloperoxidase activity against Streptococcus mutans. J. Dent. Res. 60, 831–837 (1981).
Arlandson, M. et al. Eosinophil peroxidase oxidation of thiocyanate. Characterization of major reaction products and a potential sulfhydryl-targeted cytotoxicity system. J. Biol. Chem. 276, 215–224 (2001).
Stark, G.R. On the reversible reaction of cyanate with sulfhydryl groups and the determination Of NH2-terminal cysteine and cystine in proteins. J. Biol. Chem. 239, 1411–1414 (1964).
Stark, G.R. & Smyth, D.G. The use of cyanate for the determination of NH2-terminal residues in proteins. J. Biol. Chem. 238, 214–226 (1963).
Brennan, M.L. et al. A tale of two controversies: defining both the role of peroxidases in nitrotyrosine formation in vivo using eosinophil peroxidase and myeloperoxidase-deficient mice, and the nature of peroxidase-generated reactive nitrogen species. J. Biol. Chem. 277, 17415–17427 (2002).
Zhang, R. et al. Myeloperoxidase functions as a major enzymatic catalyst for initiation of lipid peroxidation at sites of inflammation. J. Biol. Chem. 277, 46116–46122 (2002).
Kumar, A.P., Piedrafita, F.J. & Reynolds, W.F. Peroxisome proliferator-activated receptor gamma ligands regulate myeloperoxidase expression in macrophages by an estrogen-dependent mechanism involving the -463GA promoter polymorphism. J. Biol. Chem. 279, 8300–8315 (2004).
Thukkani, A.K. et al. Identification of alpha-chloro fatty aldehydes and unsaturated lysophosphatidylcholine molecular species in human atherosclerotic lesions. Circulation 108, 3128–3133 (2003).
Hörkkö, S., Savolainen, M.J., Kervinen, K. & Kesaniemi, Y.A. Carbamylation-induced alterations in low-density lipoprotein metabolism. Kidney Int. 41, 1175–1181 (1992).
Sugiyama, S. et al. Hypochlorous acid, a macrophage product, induces endothelial apoptosis and tissue factor expression: involvement of myeloperoxidase-mediated oxidant in plaque erosion and thrombogenesis. Arterioscler. Thromb. Vasc. Biol. 24, 1309–1314 (2004).
Yang, J., Cheng, Y., Ji, R. & Zhang, C. A novel model of inflammatory neointima formation reveals a potential role of myeloperoxidase in neointimal hyperplasia. Am. J. Physiol. Heart Circ. Physiol. 291, H3087–H3093 (2006).
Hill, P., Haley, N.J. & Wynder, E.L. Cigarette smoking: carboxyhemoglobin, plasma nicotine, cotinine and thiocyanate vs self-reported smoking data and cardiovascular disease. J. Chronic Dis. 36, 439–449 (1983).
Markwell, M.A., Haas, S.M., Bieber, L.L. & Tolbert, N.E. A modification of the Lowry procedure to simplify protein determination in membrane and lipoprotein samples. Anal. Biochem. 87, 206–210 (1978).
Podrez, E.A. et al. Macrophage scavenger receptor CD36 is the major receptor for LDL modified by monocyte-generated reactive nitrogen species. J. Clin. Invest. 105, 1095–1108 (2000).
Anderson, K.M., Odell, P.M., Wilson, P.W. & Kannel, W.B. Cardiovascular disease risk profiles. Am. Heart J. 121, 293–298 (1991).
Stoves, J., Lindley, E.J., Barnfield, M.C., Burniston, M.T. & Newstead, C.G. MDRD equation estimates of glomerular filtration rate in potential living kidney donors and renal transplant recipients with impaired graft function. Nephrol. Dial. Transplant. 17, 2036–2037 (2002).
Acknowledgements
Supported by US National Institutes of Health grants HL70621, P01 HL076491 and P01 HL077107 and by the Cleveland Clinic General Clinical Research Center (M01 RR018390).
Author information
Authors and Affiliations
Contributions
Z.W. performed the biochemical, cellular, animal model and mass spectrometry studies, as well as assisting in drafting the manuscript. S.J.N. assisted with clinical studies design and statistical analysis. E.R.R. performed histology studies on human atherosclerotic plaque. O.K. and S.H. generated the monoclonal antibody to carbamylated LDL. J.B. assisted with clinical trial design and statistical analyses. W.F.R. collaborated in MPO transgenic mouse studies. E.J.T. participated in acquisition of clinical data and materials. J.A.D. participated in biochemical and cell biological characterization studies of carbamylated proteins. S.L.H. conceived the idea for the study, designed experiments, drafted manuscript and provided all funding. All authors provided critical review and comments on the manuscript.
Corresponding author
Ethics declarations
Competing interests
S.L.H. is named as co-inventor on pending patents filed by the Cleveland Clinic that relate to the use of biomarkers to inflammatory and cardiovascular diseases. He is also the scientific founder and a consultant to PrognostiX Inc., and has received honoraria and consulting fees related to cardiovascular biomarkers from Abbott, BioSite, Lilly, Merck, Pfizer, Wyeth and Biophysical.
Supplementary information
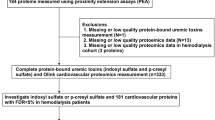
Supplementary Text and Figures
Supplementary Fig. 1, Supplementary Tables 1–4 and Supplementary Methods (PDF 610 kb)
Rights and permissions
About this article
Cite this article
Wang, Z., Nicholls, S., Rodriguez, E. et al. Protein carbamylation links inflammation, smoking, uremia and atherogenesis. Nat Med 13, 1176–1184 (2007). https://doi.org/10.1038/nm1637
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nm1637
This article is cited by
-
Analysis of a macrophage carbamylated proteome reveals a function in post-translational modification crosstalk
Cell Communication and Signaling (2023)
-
Amino acids downregulate SIRT4 to detoxify ammonia through the urea cycle
Nature Metabolism (2023)
-
Comparison of homocitrulline and carbamylated albumin as biomarkers of carbamylation reactions in hemodialyzed patients
Amino Acids (2023)
-
Age and sex differences in the risk of cardiovascular diseases by chronic kidney disease in a general Japanese population
Heart and Vessels (2023)
-
Association between environmental exposure to perchlorate, nitrate, and thiocyanate and serum α-Klotho levels among adults from the National Health and nutrition examination survey (2007–2014)
BMC Geriatrics (2022)