Abstract
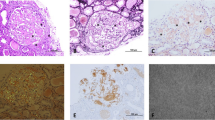
Renal amyloidosis is a rare and intractable disease that accounts for 0.2% of the original kidney diseases of dialysis patients in Japan. However, the number of patients with renal amyloidosis seems to be increasing in recent years. There have been some new concepts focusing on the mechanism of amyloidogenesis, such as molecular chaperones, seeding mechanism, and genetic polymorphisms of precursor protein. Clinical and histological features of renal amyloidosis vary according to the type. Significantly higher levels of urinary protein excretion are seen in the AL type, whereas microscopic haematuria is more prominent in the AA type. Histologically, amyloid deposition of AL type has stronger predilection for GBM than mesangium, and spicule formation is more frequently observed. In contrast, AA type has a higher affinity to TBM and interstitial area. For the histological diagnosis of renal amyloidosis, plural staining methods including Congo-red, Daylon and thioflavin-T stains are available. Combinations of these staining methods are necessary for establishing the precise diagnosis. The more recent and intensive treatments for renal amyloidosis are expected to improve patient outcome. For AL amyloidosis, high-dose melphalan plus high-dose dexamethasone or VAD, in conjunction with bone marrow stem cells transplantation, have shown a definitive effect on reducing urinary protein excretion. The biological agent, tumor necrosis factor (TNFα) blocker, improves the renal function in AA-type renal amyloidosis, as well as suppresses the inflammatory reactions in patients with rheumatoid arthritis. Clinical advances have been made in various aspects of renal amyloidosis.




Similar content being viewed by others
References
Kingman A, Pereira NLC. Ardiac amyloidosis. J S C Med Assoc 2001;97:201–6.
Kelly JJ. Neurologic complications of primary systemic amyloidosis. Rev Neurol Dis 2006;3(4):173–81.
Nestle FO, Burg G. Bilateral carpal tunnel syndrome as a clue for the diagnosis of systemic amyloidosis. Dermatology 2001;202:353–5.
Alhaddab M, Srolovitz H, Rosen N. Primary systemic amyloidosis presenting as extensive cutaneous ulceration. J Cutan Med Surg 2006;10:253–6.
Kyle RA. Plasma cell disorderes. In: Glodman L, Bennett JC, editor. Cecil textbook of medicine. 21st. 2000;977–87.
Kyle RA, Wagoner RD, Holley KE. Primary systemic amyloidosis: resolution of the nephrotic syndrome with melphalan and prednisone. Arch Intern Med 1982;142:1445–7.
Goddard IR, Jackson R, Jones JM. AL amyloidosis: therapeutic response in two patients with renal involvement. Nephrol Dial Transplant 1991;6:592–4.
Kyle RA, Gertz MA, Greipp PR, Witzig TE, Lust JA, Lacy MQ, et al. A trial of three regimens for primary amyloidosis: colchicine alone, melphalan and prednisone, and melphalan, prednisone, and colchicine. N Engl J Med 1997;336:1202–7.
Comenzo RL, Vosburgh E, Falk RH, Sanchorawala V, Reisinger J, Dubrey S, et al. Dose-intensive melphalan with blood stem-cell support for the treatment of AL (amyloid light-chain) amyloidosis: survival and responses in 25 patients. Blood 1998;91:3662–70.
Ravindran J, Shenker N, Bhalla AK, Lachmann H, Hawkins P. Case report: Response in proteinuria due to AA amyloidosis but not Felty’s syndrome in a patient with rheumatoid arthritis treated with TNF-alpha blockade. Rheumatology (Oxford) 2004;43:669–72.
Bergesio F, Ciciani AM, Santostefano M, Brugnano R, Manganaro M, Palladini G, et al. Renal involvement in systemic amyloidosis—an Italian retrospective study on epidemiological and clinical data at diagnosis. Dial Transplant 2007;29:[Epub ahead of print].
Esteve V, Almirall J, Ponz E, Garcia N, Ribera L, Larrosa M, et al. Renal involvement in amyloidosis. Clinical outcomes, evolution and survival. Nefrologia 2006;26:212–7.
Ensari C, Ensari A, Tumer N, Ertug E. Clinicopathological and epidemiological analysis of amyloidosis in Turkish patients. Nephrol Dial Transplant 2005;20:1721–5.
Mehta HJ, Talwalkar NC, Merchant MR, Mittal BV, Suratkal LH, Almeida AF, et al. Pattern of renal amyloidosis in western India. A study of 104 cases. J Assoc Physicians India 1990;38:407–10.
Singh R, Singh MM, Lahiri VL, Mirchandani HM. Tuberculosis as a continuing cause of secondary amyloidosis in northern India. J Indian Med Assoc 1987;85:328–32.
Gallo G, Wisniewski T, Choi-Miura NH, Ghiso J, Frangione B. Potential role of apolipoprotein-E in fibrillogenesis. Am J Pathol 1994;145:526–30.
Coker AR, Purvis A, Baker D, Pepys MB, Wood SP. Molecular chaperone properties of serum amyloid P component. FEBS Lett 2000;473:199–202.
Westermark P. Aspects on human amyloid forms and their fibril polypeptides. FEBS J 2005;272:5942–9.
Takahashi N, Hasegawa K, Yamaguchi I, Okada H, Ueda T, Gejyo F, et al. Establishment of a first-order kinetic model of light chain-associated amyloid fibril extension in vitro. Biochim Biophys Acta 2002;1601:110–20.
Naiki H, Gejyo F. Kinetic analysis of amyloid fibril formation. Methods Enzymol 1999;309:305–18.
Yamaguchi I, Hasegawa K, Takahashi N, Gejyo F, Naiki H. Apolipoprotein E inhibits the depolymerization of beta 2-microglobulin-related amyloid fibrils at a neutral pH. Biochemistry 2001;40:8499–507.
Booth DR, Booth SE, Gillmore JD, Hawkins PN, Pepys MB. SAA1 alleles as risk factors in reactive systemic AA amyloidosis. Amyloid. 1998;5:262–5.
Yamada T, Wada A, Itoh Y, Itoh K. Serum amyloid A1 alleles and plasma concentrations of serum amyloid A. Amyloid. 1999;6:199–204.
Moriguchi M, Kaneko H, Terai C, Koseki Y, Kajiyama H, Inada S, et al. Relative transcriptional activities of SAA1 promoters polymorphic at position -13(T/C): potential association between increased transcription and amyloidosis. Amyloid 2005;12:26–32.
Yamada T, Okuda Y, Takasugi K, Wang L, Marks D, Benson MD, et al. An allele of serum amyloid A1 associated with amyloidosis in both Japanese and Caucasians. Amyloid 2003;10:7–11.
Ajiro J, Narita I, Sato F, Saga D, Hasegawa H, Kuroda T, et al. SAA1 gene polymorphisms and the risk of AA amyloidosis in Japanese patients with rheumatoid arthritis. Mod Rheumatol 2006;16:294–9.
Kyle RA, Therneau TM, Rajkumar SV, Larson DR, Plevak MF, Offord JR, et al. Prevalence of monoclonal gammopathy of undetermined significance. N Engl J Med 2006;354:1362–9.
Kyle RA, Rajkumar SV. Monoclonal gammopathies of undetermined significance: a review. Immunol Rev 2003;194:112–39.
Kyle RA, Rajkumar SV. Monoclonal gammopathy of undetermined significance. Clin Lymphoma Myeloma 2005;6:102–14.
Katzmann JA, Clark RJ, Abraham RS, Bryant S, Lymp JF, Bradwell AR, et al. Serum reference intervals and diagnostic ranges for free kappa and free lambda immunoglobulin light chains: relative sensitivity for detection of monoclonal light chains. Clin Chem 2002;48:1437–44.
Abraham RS, Katzmann JA, Clark RJ, Bradwell AR, Kyle RA, Gertz MA, et al. Quantitative analysis of serum free light chains. A new marker for the diagnostic evaluation of primary systemic amyloidosis. Am J Clin Pathol 2003;119:274–8.
Katzmann JA, Abraham RS, Dispenzieri A, Lust JA, Kyle RA. Diagnostic performance of quantitative kappa and lambda free light chain assays in clinical practice. Clin Chem 2005;51:878–81.
Katzmann JA, Dispenzieri A, Kyle RA, Snyder MR, Plevak MF, Larson DR, et al. Elimination of the need for urine studies in the screening algorithm for monoclonal gammopathies by using serum immunofixation and free light chain assays. Mayo Clin Proc 2006;81:1575–8.
Akpolat T, Diri B, Oguz Y, Yilmaz E, Yavuz M, Dilek M, et al. Behcet’s disease and renal failure. Nephrol Dial Transplant 2003;18:888–91.
Nakano M, Ueno M, Nishi S, Shimada H, Hasegawa H, Watanabe T, et al. Analysis of renal pathology and drug history in 158 Japanese patients with rheumatoid arthritis. Clin Nephrol 1998;50:154–60.
Dember LM. Amyloidosis-associated kidney disease. J Am Soc Nephrol 2006;17:3458–71.
Ferrario F, Rastaldi MP. Renal amyloidosis (Part II). J Nephrol 2006;19:242–5.
Bohle A, Wehrmann M, Eissele R, von Gise H, Mackensen-Haen S, Muller C. The long-term prognosis of AA and AL renal amyloidosis and the pathogenesis of chronic renal failure in renal amyloidosis. Pathol Res Pract 1993;189:316–31.
Sasatomi Y, Sato H, Chiba Y, Abe Y, Takeda S, Ogahara S, et al. Prognostic factors for renal amyloidosis: a clinicopathological study using cluster analysis. Intern Med 2007;46:213–9.
Osawa Y, Kawamura K, Kondo D, Imai N, Ueno M, Nishi S, et al. Renal function at the time of renal biopsy as a predictor of prognosis in patients with primary AL-type amyloidosis. Clin Exp Nephrol 2004;8:127–33.
Kuroda T, Tanabe N, Harada T, Murakami S, Hasegawa H, Sakatsume M, et al. Long-term mortality outcome in patients with reactive amyloidosis associated with rheumatoid arthritis. Clin Rheumatol 2006;25:498–505.
Kuroda T, Tanabe N, Sakatsume M, Nozawa S, Mitsuka T, Ishikawa H, et al. Comparison of gastroduodenal, renal and abdominal fat biopsies for diagnosing amyloidosis in rheumatoid arthritis. Clin Rheumatol. 2002;21:123–8.
Ansari-Lari MA, Ali SZ. Fine-needle aspiration of abdominal fat pad for amyloid detection: a clinically useful test? Diagn Cytopathol 2004;30:178–81.
Hachulla E, Grateau G. Diagnostic tools for amyloidosis. Joint Bone Spine 2002;69:538–45.
Gomez-Casanovas E, Sanmarti R, Sole M, Canete JD, Munoz-Gomez J. et al. The clinical significance of amyloid fat deposits in rheumatoid arthritis: a systematic long-term followup study using abdominal fat aspiration. Arthritis Rheum 2001;44:66–72.
Mcalpine JC, Bancroft JD. A histological study of hyaline deposits in laryngeal, aural, and nasal polyps and their differentiation from amyloid. J Clin Pathol 1964;17:213–9.
Puchtler H, Waldrop FS, Meloan SN. A review of light, polarization and fluorescence microscopic methods for amyloid. Appl Pathol 1985;3:5–17.
Elghetany MT, Saleem A, Barr K. The congo red stain revisited. Ann Clin Lab Sci 1989;19:190–5.
Puchtler H, Sweat Waldrop F, Meloan SN. Application of thiazole dyes to amyloid under conditions of direct cotton dyeing: correlation of histochemical and chemical data. Histochemistry 1983;77:431–45.
Takahashi T, Miura H, Matsu-ura Y, Iwana S, Maruyama R, Harada T. Urine cytology of localized primary amyloidosis of the ureter: a case report. Acta Cytol 2005;49:319–22.
Iijima S. Primary systemic amyloidosis: a unique case complaining of diffuse eyelid swelling and conjunctival involvement. J Dermatol 1992;19:113–8.
Stiller D, Katenkamp D, Thoss K. Staining mechanism of thioflavin T with special reference to the localization of amyloid. Acta Histochem 1972;42:234–45.
Nebut M, Hartmann L. Contribution of thioflavin T in the study of the early histologic lesions of experimental amyloidosis. Ann Biol Clin 1966;24:1063–79.
Rogers DR. Screening for amyloid with the thioflavin-T fluorescent method. Am J Clin Pathol 1965;44:59–61.
Korpela M, Mustonen J, Teppo AM, Helin H, Pasternack A. Mesangial glomerulonephritis as an extra-articular manifestation of rheumatoid arthritis. Br J Rheumatol 1997;36:1189–95.
Nakano M, Ueno M, Nishi S, Suzuki S, Hasegawa H, Watanabe T, et al. Determination of IgA- and IgM-rheumatoid factors in patients with rheumatoid arthritis with and without nephropathy. Ann Rheum Dis 1996;55:520–4.
Korpela M, Mustonen J, Helin H, Pasternack A. Immunological comparison of patients with rheumatoid arthritis with and without nephropathy. Ann Rheum Dis 1990;49:214–8.
Shirahama T, Cohen AS. High-resolution electron microscopic analysis of the amyloid fibril. J Cell Biol 1967;33:679–708.
Dember LM. Amyloidosis-associated kidney disease. J Am Soc Nephrol 2006;17:3458–71.
Nishi S, Ogino S, Maruyama Y, Honma N, Gejyo F, Morita T, et al. Electron-microscopic and immunohistochemical study of beta-2-microglobulin-related amyloidosis. Nephron 1990;56:357–63.
Yang GC, Gallo GR. Protein A-gold immunoelectron microscopic study of amyloid fibrils, granular deposits, and fibrillar luminal aggregates in renal amyloidosis. Am J Pathol 1990;137:1223–31.
Shiiki H, Shimokama T, Yoshikawa Y, Toyoshima H, Kitamoto T, Watanabe T. Renal amyloidosis. Correlations between morphology, chemical types of amyloid protein and clinical features. Virchows Arch A Pathol Anat Histopathol 1988;412:197–204.
Watanabe T, Saniter T. Morphological and clinical features of renal amyloidosis. Virchows Arch A Pathol Anat Histol 1975;366:125–35.
Shiiki H, Shimokama T, Yoshikawa Y, Onoyama K, Morimatsu M, Watanabe T. Perimembranous-type renal amyloidosis: a peculiar form of AL amyloidosis. Nephron. 1989;53:27–32.
Sasatomi Y, Sato H, Chiba Y, Abe Y, Takeda S, Ogahara S, et al. Prognostic factors for renal amyloidosis: a clinicopathological study using cluster analysis. Intern Med. 2007;46(5):213–9.
Sezer O, Schmid P, Shweigert M, Heider U, Eucker J, Harder H, et al. Rapid reversal of nephrotic syndrome due to primary systemic AL amyloidosis after VAD and subsequent high-dose chemotherapy with autologous stem cell support. Bone Marrow Transplant 1999;23:967–9.
Dember LM, Sanchorawala V, Seldin DC, Wright DG, LaValley M, Berk JL, et al. Effect of dose-intensive intravenous melphalan and autologous blood stem-cell transplantation on al amyloidosis-associated renal disease. Ann Intern Med 2001;134:746–53.
Sanchorawala V, Wright DG, Seldin DC, Dember LM, Finn K, Falk RH, et al. An overview of the use of high-dose melphalan with autologous stem cell transplantation for the treatment of AL amyloidosis. Bone Marrow Transplant 2001;28:637–42.
Perfetti V, Siena S, Palladini G, Bregni M, Di Nicola M, Obici L, et al. Long-term results of a risk-adapted approach to melphalan conditioning in autologous peripheral blood stem cell transplantation for primary (AL) amyloidosis. Haematologica 2006;91:1635–43.
Smith GR, Tymms KE, Falk M. Etanercept treatment of renal amyloidosis complicating rheumatoid arthritis. Intern Med J 2004;34:570–2.
Rysava R, Merta M, Spicka I, Tesar V. Current therapeutic possibilities in primary and secondary amyloidosis and our experience with 31 patients. Nephrol Dial Transplant 2003;18(Suppl 5):38–40.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Nishi, S., Alchi, B., Imai, N. et al. New advances in renal amyloidosis. Clin Exp Nephrol 12, 93–101 (2008). https://doi.org/10.1007/s10157-007-0008-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-007-0008-3