Abstract
Objective
To evaluate the impact of the coronavirus disease 2019 (COVID-19) pandemic on rheumatology practice.
Method
A cross-sectional web survey was designed by the members of the Arab League of Associations for Rheumatology (ArLAR), validated by its scientific committee and disseminated through e-mail and social media. It included close-ended questions about the impact of the pandemic on the rheumatology activities, including outpatient visits and hospitalizations (in percentage, 100% corresponds to complete suspension) and open-ended questions about unmet needs. Univariate and multivariable logistic regression analyses were used to evaluate the predictors of impact. Suggestions were developed to improve the practice.
Results
A total of 858 rheumatologists were included in the analysis (27.3% of registered in ArLAR), 37% were 35–44 years old, 60% were females, and 48% worked in the private sector. The impact of COVID-19 was a decrease of 69% in hospitalizations, 65% in outpatient clinic, 56% in infusion centers, and 43% in income. It was associated with the region (highest in the Gulf), use of telemedicine, impact on income and practice sector (lowest in private). There was a hydroxychloroquine shortage in 47%. Telemedicine was mostly based on traditional telephone contacts and e-mails and reimbursed in 12%. Fifteen rheumatologists (1.8%) were infected and 156 cases of COVID-19 were reported among patients. The top-cited unmet needs in rheumatology practice were access to drugs and a telemedicine platform.
Conclusions
The negative impact of the COVID-19 pandemic on rheumatology practice may compromise rheumatic diseases control. Better access to drugs and providing telemedicine platforms are recommended to improve the practice.
Key Points • The COVID-19 pandemic had a significant negative impact on the rheumatology practice, including access to outpatient clinic, hospitalization, and to anchor drugs. • The compromised access to rheumatology care may jeopardize the control of chronic rheumatic diseases and the long-term prognosis. • Better access to drugs and providing telemedicine platforms are strongly recommended. |
Similar content being viewed by others

Introduction
The coronavirus disease 2019 (COVID-19) has emerged in December 2019 in Wuhan, China, to quickly become a global outbreak and a significant public health issue [1, 2]. On January 30, 2020, the World Health Organization (WHO) declared COVID-19 a public health emergency of international concern [3], and on March 20, 2020, due to the devastating number of new cases reported globally, WHO declared it as a pandemic [4]. At the time of drafting this manuscript (June 28, 2020), the WHO reported more than 9.5 million COVID-19 cases and 495,760 deaths [5].
During the pandemic, health care professionals (HCP) were faced with many challenges in the fight against an unprecedented and rapidly spreading disease [4]. This has prompted the WHO and the Centers for Disease Control and Prevention (CDC) to publish recommendations for the prevention and control of COVID-19 for HCP by the end of January 2020 [6, 7].
In addition to disruptions due to the lockdown and the social distancing constraints [8, 9], the rheumatology practice had to face additional challenges.
The medical community was uncertain if immunocompromised patients with rheumatic diseases had a higher risk of infection with the novel severe acute respiratory syndrome coronavirus (SARS-CoV-2) [10,11,12,13,14,15,16]. Several recommendations were developed worldwide to guide the rheumatologists in their therapeutic choices [17,18,19,20,21,22]. However, the decision to stop, pursue, or initiate therapies had to be determined, sometimes remotely, on a case-by-case basis, according to clinical judgment. In some cases, patients even decided to modify their treatment on their own without notifying their physician [23].
Moreover, some symptoms and signs may be overlapping between COVID-19 and immune-mediated disease flares [13, 15], which may cause diagnostic confusion in some cases and difficulties in making therapeutic decisions [24].
Furthermore, several rheumatology drugs were thought to have potential activity against the SARS-CoV-2, especially hydroxychloroquine (HCQ), thus leaving the rheumatology patients in drug shortage sometimes [25,26,27].
Finally, rheumatologists were regularly solicited by chronic patients for advice and by colleagues for assistance in rheumatology drugs prescription for COVID-19 cytokine storm management [28, 29], which could be mentally draining.
Therefore, COVID-19 pandemic is a truly challenging time for rheumatologists, particularly in the Arab countries. Unlike the USA or Western Europe [30, 31], the concept of telemedicine is not well established in the Arab world. The main obstacles include the absence of a legal telemedicine framework and the reluctance of patients to renounce their privileged physician-patient direct communication. For this purpose, rheumatologists from the Arab League of Associations for Rheumatology (ArLAR) designed a survey to evaluate the difficulties faced by the rheumatologists in the Arab countries.
Objectives
The primary objective was to evaluate the impact of COVID-19 pandemic on rheumatology practice in the Arab countries.
The secondary objectives were to evaluate the impact of COVID-19 on the rheumatologists themselves and to develop suggestions to improve the rheumatology practice in the region.
Method
A 21-item web-based, cross-sectional survey was developed by a steering committee comprising rheumatologists from the ArLAR. The survey was designed in English, based on the available literature, and following the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) guidelines [32]. It was validated by the ArLAR scientific committee, which consists of rheumatologists representing all 15 ArLAR countries.
The survey instrument was also translated and validated in French by the steering committee. A pilot test was run in both languages with six bilingual rheumatologists to evaluate the timing, readability, relevance, and acceptability. The questionnaire was considered easy to read, relevant and acceptable, and required around 3 min to complete.
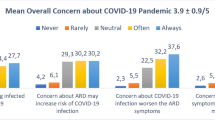
The survey comprised 19 close-ended and simple numeric questions about the demographic characteristics, the impact of the pandemic on the rheumatology activity (outpatient visits, day and regular hospitalization) and practice income (expressed in percentages, where 0% corresponds to the absence of impact, and 100% corresponds to a complete suspension of activities), the direct impact on the personal life of the rheumatologists including personal infection with SARS-CoV-2, the impact on mental health (using a simple question), the attitude towards telemedicine, as well as two open-ended questions about the unmet needs and the ways to improve the current practice (Supplementary data 1).
Both versions, in English and French, were made accessible through a Google form link. The survey was disseminated to all the rheumatologists working in the 15 ArLAR countries through the ArLAR mass mailing system, with a prospective data collection between May 9 and May 24, 2020. It was also advertised on ArLARs’ and Arab rheumatology societies’ social media (Facebook, Twitter, and Instagram) for 16 days. The study was named HARMONIC (How are the Arab RheuMatologists dealiNg with the COVID-19 pandemIC) on social media. Participation through Google forms was anonymous.
Based on the survey results, the authors developed a set of suggestions to help improve the rheumatology practice across the Arab countries.
Consent to participate and ethical considerations
The rheumatologists received the invitation to participate by mass e-mail through the ArLAR. Clicking on the button “fill out the form” was considered the equivalent of consent to participate in the survey. Confidentiality of personal information was maintained throughout the study by making participants’ information anonymous. The study was approved by the Saint-Joseph University Ethics Committee (number CEHDF 1654).
Statistical analysis
The number of rheumatologists in the participating countries is estimated to be around 3137 rheumatologists. We aimed at including around 25% of this total (600). Moreover, for the analysis, the countries of practice (societies registered in ArLAR) were grouped into three geographical regions, i.e., Levant (Iraq, Jordan, Lebanon, Palestine, Syria), Gulf (Kingdom of Saudi Arabia (KSA), Kuwait, Oman, Qatar, United Arab Emirates (UAE)), and North Africa (Algeria, Egypt, Libya, Morocco, Tunisia).
Continuous variables were expressed by mean and standard deviation and categorical variables as numbers and percentages. Comparison of the rheumatologists’ characteristics and responses between the three regions was performed using the Pearson chi-square or Fisher test for the categorical variables and the t test or ANOVA for the continuous variables.
Furthermore, the dependent variable “impact on clinical activity” was categorized into a binary variable—higher impact and lower impact, using the median as a cut-off. Univariate and multivariable binary logistic regression analyses were conducted to identify factors associated with this dependent variable. All independent variables with a p value ˂ 0.1 in the univariate analysis were taken into account in the multivariable logistic regression analysis; p values < 0.05 were accepted as statistically significant. All statistical analyses were performed using SPSS v23 (IBM).
The results of the open-ended items were analyzed and assembled into themes. Discordances were resolved through discussion.
Results
Descriptive analysis of the HARMONIC study participants
Out of the 3137 rheumatologists registered in the 15 ArLAR societies, 1214 clicked on the survey link, and 865 responded to the survey (Fig. 1, flowchart of the participants). Seven responses reported a non-Arab current country of practice and were eliminated. Therefore, a total of 858 rheumatologists were included in the analysis (26.9% of the total number of registered rheumatologists in ArLAR).
Among these participants, 37% were in the 35–44 years age group. The rheumatologists had been practicing rheumatology for 13.4 years (SD 9.7). Sixty percent were females. Forty-eight percent of the participants worked in private sectors, and 45% worked in university hospitals; notably, 267 rheumatologists (31%) worked in more than one practice sector. Thirty-nine percent worked in institutions that were implicated in the frontline management of COVID-19, and 22% were personally involved in the frontline management of the pandemic. There were significant differences between the Levant, Gulf, and North Africa. The participants’ characteristics by region are presented in Table 1 and their participation rate by country in Supplementary data 2.
Impact of the COVID-19 pandemic on the rheumatology practice
The impact of the COVID-19 pandemic on the outpatient visits was estimated to be a 65% decrease in activities, highest in the Gulf (76%) and lowest in the Levant (53%) (p < 0.001). The impact was a 56% decrease in day hospital (infusion centers) and a 69% decrease in regular hospitalization, both lowest in the Gulf and highest in North Africa. The impact of the pandemic on the practice income was a 43% decrease, which was highest in the Levant (50%) and lowest in the Gulf (27%) (Table 2).
The impact on the outpatient clinic activity was categorized into higher versus lower impact, using the median, 70%, as a cut-off. In univariate analysis, a higher impact was associated with age (p < 0.001), region (p < 0.001), private sector of activity (p < 0.001), using telemedicine (p < 0.001), institution implicated in COVID-19 (p < 0.004), frontline management of COVID-19 (p = 0.009), patient with COVID-19 death (p = 0.001), personal infection with SARS-CoV-2 (p = 0.022), and impact on income (p < 0.001). In multivariable analysis, the region (higher impact in the Gulf, followed by North Africa then the Levant) and using telemedicine remained associated with a higher impact on the clinic activity, whereas working in the private sector was associated with a lower impact on the clinical activity (compared with working in the public sector and in university teaching hospital) (Table 3).
Impact of the COVID-19 pandemic on the logistics of the practice
During the visit to the outpatient clinic, 98.3% of the rheumatologists used additional precautions: 93.4% used masks for themselves, 60.7% used masks for the patients, 66.6% used gloves for themselves, 15.4% used gloves for the patients and 78.2% used more antiseptics (hand sanitizers, surface antiseptics) than usual.
Because of the pandemic, there was a shortage of HCQ in 47% of cases (highest in North Africa (61.2%) and lowest in the Levant (26.1%) (p < 0.001)). Also, there was a difficulty in accessing HCQ in an additional 24.2% of cases (Table 2).
Telemedicine
Regarding the practice of telemedicine, the rheumatologists reported to use it in 70% of the cases, i.e., as a full facility in 10%, as a partial facility in 16%, and in more traditional ways (telephone, e-mails) in 51% of cases, with a higher telemedicine practice in the Gulf (p < 0.001). Telemedicine was reimbursed in 22% of cases in the Gulf, 10% in the Levant, and 8% in North Africa (12% in total) (Table 2). As for the agreement to use telemedicine, 54% fully agree to use it, 24% would agree if it is reimbursed, and 22% do not agree to use it.
Impact of the COVID-19 pandemic on the rheumatologists
The mental impact related to the stress caused by COVID-19 was reported in 77% of the respondents. It was minor in 60.4% and major in 16.7% of cases. It was numerically higher in North Africa (80.2% of cases), but the difference between the regions was not statistically significant (p = 0.158) (Table 2).
Twenty-five percent of the rheumatologists felt they were totally prepared in case they were asked to work in the frontline management of COVID-19, 45% felt partially prepared, whereas 30% were not prepared at all. Preparedness was highest in the Gulf (86%) and lowest in North Africa (58%), p < 0.001.
Infection with SARS-CoV-2
Fifteen rheumatologists (1.8%) reported that they were personally infected with SARS-CoV-2, five in each of the 3 regions. One-third (5) of these rheumatologists were involved in the management of COVID-19 as frontline physicians. Also, 34 rheumatologists (3.96%) said they were in quarantine because of COVID-19, 22 of which were from the Levant.
As for the rheumatology patients infected with SARS-Cov-2, 156 cases were reported by the rheumatologists (51 from the Gulf, 48 from the Levant, and 57 from North Africa). Of these 156 cases, 32 (20.5%) were treated in ambulatory, 59 (37.8%) were hospitalized, 22 (14.1%) were admitted to the intensive care unit, and 35 (22.4%) died. The outcome was unknown in 33 (21.1%) cases.
Unmet needs and ways to improve the practice
In the open-ended questions, 349 rheumatologists provided 509 comments about the unmet needs in the rheumatology practice in the Arab countries, and 294 rheumatologists provided 565 comments about the way to improve this practice. After the classification of the answers into themes, the top-cited needs and possible ways of improvement were as follows: access to drugs (biologics and HCQ), a telemedicine platform, an organized rheumatology unit, personal protective equipment (PPE), patient education, continuous medical education for physicians, and advocacy for rheumatology (the ranking of the top five unmet needs related to the pandemic is presented in Table 4).
Based on the open-ended responses, the steering committee developed suggestions to improve the rheumatology practice during the pandemic and in the deconfinement period (Table 4). The authors highlighted the need for local guidance for rheumatologists and patients, for working with health authorities to guarantee the availability of drugs for patients and PPE for HCP, and for establishing a reliable telemedicine platform that will help to rationalize human resources, reduce infection risk, and ensure the proper continuity of rheumatology care.
Discussion
The current study showed a significant negative impact of the COVID-19 pandemic on the rheumatology practice. The impact was higher on the regular hospitalization, followed by the outpatient clinic and the daily hospitalization for infusion. The differences in the impact between the Levant, the Gulf, and North Africa are partly due to differences in the healthcare system (more private-based in the Levant, more public-based in the Gulf), as well as differences in the pandemic response pattern (earlier and more strict quarantine measures in the Gulf and North Africa, compared with the Levant).
This significant negative impact on the continuity of rheumatology care, coupled with the shortage in some cornerstone drugs, such as HCQ (47% in the current study), may have a substantial impact on the control of chronic rheumatic diseases, putting the patients at a high risk of disease flare and compromising the disease prognosis on the short and long term [33].
The impact on the practice also translated into a 43% impact on the income, reflecting the serious economic repercussions of the pandemic. This economic impact of the pandemic is global, as announced by a United Nations Conference on Trade and Development report [34]. Nevertheless, it is different from one country to another (lowest in the Gulf countries), reflecting the baseline socio-economic disparities between the countries.
A higher impact on the outpatient clinic was associated with higher use of telemedicine, probably to compensate for the compromised access of the patient to rheumatology care. However, telemedicine was mostly used in a “traditional way,” such as telephone or e-mail contact, which cannot replace a regular visit in rheumatology, and may not be sustainable in the long term. The lack of appropriate compensation (12%) contributes probably to the reluctance of about half of the rheumatologists if implementing it in their practice.
The mental impact of the pandemic was also considerable, as 77% of the respondents had some sort of impact. This is expected, as healthcare professionals, in general, are faced with additional challenges during the pandemic, such as mental stress, physical exhaustion, separation from families, stigma, risk of personal infection, and the pain of losing patients and colleagues. In the current study, 22% of the rheumatologists were implicated in the frontline management of COVID-19, and 39% worked in frontline institutions, meaning that even in a non-frontline specialty, physicians were highly implicated in the pandemic management.
The proportion of rheumatologists’ infection with SARS-CoV2 was 1.8%, which may increase with time, as the pandemic evolves. Although this number may be underestimated, since the seriously infected rheumatologists may not be able to respond to this survey, it gives a preliminary estimate about the direct proportion of infection among the rheumatologists, as this information is still lacking worldwide.
As for the reported patients’ infection, a high mortality rate (22% of the 156 reported cases) was noted in comparison with the figures reported by the COVID-19 Global Rheumatology Alliance physician-reported registry (9%) [13] and in cohort of patients with chronic rheumatic diseases from Spain and Italy (6 to 10%) [16, 35]. This result mostly reflects a bias towards more severe cases that “come to the attention” of rheumatologists, relative to increased mortality. It highlights the need to involve the rheumatologist in the management of rheumatic patients who are affected by COVID-19. Also, this bias may be due to the fact that only individuals with severe symptoms are being tested for COVID-19 in most Arab countries.
Based on the results of this survey, the developed suggestions by the steering committee will be used to improve the rheumatology practice during the pandemic and in the deconfinement period. Although international recommendations are published, having local guidance based on the Arab region’s specific unmet needs is of utmost importance in the current pandemic.
The study has some limitations. The questionnaire was developed de novo, based on the available literature. However, it was validated by an independent scientific committee and pilot-tested successfully for readability, acceptability, and timing.
Also, the study was cross-sectional, covering a period where the pandemic had already reached its peak in some countries, whereas it was still in the ascending part of the curves in others. Therefore, the responses reflect the status in each country in a particular time frame of the pandemic. Also, the young age of the participants reflect the users of social media in the Arab region [36] and may jeopardize the external validity of the study.
Besides, the data presented in this study were self-reported and partly dependent on recall ability; thus, they may carry subjectivity and recall bias. Moreover, duplicate data, although very unlikely, cannot be ruled out as multiple entries could not be restricted. However, not collecting personal identification data was a choice that the authors had to make it to favor anonymity. Finally, stress was self-reported using a simple question and not a validated tool of assessment.
Nevertheless, the current study provides new valuable information about the impact of COVID-19 on the rheumatology practice in the Arab regions. Although many studies have addressed the patients’ condition during the pandemic, data on physicians and practice remain very limited. The current study has gathered significant information from 27% of all rheumatologists across 15 Arab countries. It was disseminated in two languages, catching the broadest audience in the region, as most Arab countries study and practice medicine in English and French. Also, the study presented the first estimates about the proportion of SARS-Cov-2 infection in rheumatologists, highlighting their personal risk even if they are not “traditional frontliners.” Moreover, it has presented the outcomes of patients with COVID-19 in the Arab regions for the first time, highlighting the need to involve the rheumatologists in the management of their affected patients. Finally, the results allowed the development of local suggestions to improve the rheumatology practice during the COVID-19 pandemic and for the deconfinement period, based on the specific region’s unmet needs.
Conclusion
The current study highlights the deleterious consequences of the COVID-19 pandemic on the rheumatology practice by compromising the access to clinical care and to fundamental drugs, which is expected to affect the rheumatic disease control significantly. Suggestions were developed to improve practice and include developing unified local guidelines for the rheumatologists and the patients. The health authorities are asked to guarantee access of patients to their medications and to establish reliable telemedicine platforms.
Data availability
Data can be made available upon request from the corresponding author.
References
Wu Z, McGoogan JM (2020) Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA - J Am Med Assoc 323:1239–1242. https://doi.org/10.1001/jama.2020.2648
Tang D, Comish P, Kang R (2020) The hallmarks of COVID-19 disease. PLoS Pathog 16:e1008536. https://doi.org/10.1371/journal.ppat.1008536
Team EE (2020) World Health Organization declares novel coronavirus (2019-nCoV) sixth public health emergency of international concern. Euro Surveill 25:2019–2020. https://doi.org/10.2807/1560-7917.ES.2020.25.5.200131e
WHO (2020) World Health Organization. WHO announces COVID-19 outbreak a pandemic. http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic. Accessed 28 Jun 2020
WHO (2020) WHO COVID-19 Dashboard. https://covid19.who.int/?gclid=CjwKCAjwq832BRA5EiwACvCWsUXTxEZePK3xTjFXswIn7L0b_rm1mt5LGtFld8qQ3YKGqVk_I159qhoCyxcQAvD_BwE. Accessed 31 May 2020
WHO (2019) Coronavirus disease. World Heal Organ 2020:2633. https://doi.org/10.1001/jama.2020.2633
Prevention C for DC and (2020) HAN: Update and Interim Guidance on Outbreak of 2019 Novel Coronavirus (2019-nCoV). CDC Heal Alert Netw 1–5
Wendy Parmet MS (2020) Covid-19—the law and limits of quarantine. N Engl J Med:1–2. https://doi.org/10.1056/NEJMp2009027
Rose C (2020) Am I part of the cure or am I part of the disease? Keeping coronavirus out when a doctor comes home. N Engl J Med 382:1684–1685. https://doi.org/10.1056/NEJMp2004768
Favalli EG, Agape E, Caporali R (2020) Incidence and clinical course of COVID-19 in patients with connective tissue diseases: a descriptive observational analysis. J Rheumatol Jrheum:200507. https://doi.org/10.3899/jrheum.200507
Monti S, Balduzzi PDS (2020) Clinical course of COVID-19 in a series of patients with chronic arthritis treated with immunosuppressive targeted therapies. Ann Rheum Dis 79:667–668. https://doi.org/10.1002/lt.25756
Gianfrancesco MA, Hyrich KL, Gossec L, Strangfeld A, Carmona L, Mateus EF, Sufka P, Grainger R, Wallace Z, Bhana S, Sirotich E, Liew J, Hausmann JS, Costello W, Robinson P, Machado PM, Yazdany J, COVID-19 Global Rheumatology Alliance Steering Committee (2020) Rheumatic disease and COVID-19: initial data from the COVID-19 Global Rheumatology Alliance provider registries. Lancet Rheumatol 9913:19–21. https://doi.org/10.1016/S2665-9913(20)30095-3
Gianfrancesco M, Hyrich KL, Adely SA et al (2020) Characteristics associated with hospitalisation for COVID-19 in people with rheumatic disease: data from the COVID-19 Global Rheumatology Alliance physicianreported registry. Ann Rheum Dis:1–8. https://doi.org/10.1136/annrheumdis-2020-217871
Möhn N, Pul R, Kleinschnitz C et al (2020) Implications of COVID-19 outbreak on immune therapies in multiple sclerosis patients—lessons learned from SARS and MERS. Front Immunol 11. https://doi.org/10.3389/fimmu.2020.01059
Ye C, Cai S, Shen G et al (2020) Clinical features of rheumatic patients infected with COVID-19 in Wuhan, China. Ann Rheum Dis:1–7. https://doi.org/10.1136/annrheumdis-2020-217627
D’Silva KM, Serling-Boyd N, Wallwork R, Hsu T, Fu X, Gravallese EM, Choi HK, Sparks JA, Wallace ZS (2019) Clinical characteristics and outcomes of patients with coronavirus disease 2019 (COVID-19) and rheumatic disease: a comparative cohort study from a US “hot spot”. Ann Rheum Dis 2020:1–7. https://doi.org/10.1136/annrheumdis-2020-217888
Mikuls TR, Johnson SR, Fraenkel L et al (2020) American College of Rheumatology guidance for the management of adult patients with rheumatic disease during the COVID-19 pandemic. Arthritis Rheumatol:41301. https://doi.org/10.1002/art.41301
Rheumatology AC of ACR Infusion Guidance During COVID-19 Crisis. www.rheumatology.org. Accessed 30 Apr 2020
European league against rheumatism (2020) EULAR Guidance for patients COVID-19 outbreak. https://www.eular.org/eular_guidance_for_patients_covid19_outbreak.cfm
England NHS (2020) Clinical guide for the management of Rheumatology patients during the coronavirus pandemic. Nhs:1–16
Schulze-Koops H, Specker C, Iking-Konert C, et al (2020) Preliminary recommendations of the German Society of Rheumatology (DGRh eV) for the management of patients with inflammatory rheumatic diseases during the SARS-CoV-2/Covid-19 pandemic. Ann Rheum Dis 0:1–2. https://doi.org/10.1136/annrheumdis-2020-217628
Shanthanna H, Strand NH, Provenzano DA et al (2020) Caring for patients with pain during the COVID-19 pandemic: consensus recommendations from an international expert panel. Anaesthesia:1–10. https://doi.org/10.1111/anae.15076
Michaud K, Wipfler K, Shaw Y, Simon TA, Cornish A, England BR, Ogdie A, Katz P (2020) Experiences of patients with rheumatic diseases in the US during early days of the COVID-19 pandemic. ACR Open Rheumatol 0:1–9 . https://doi.org/10.1002/acr2.11148, 2
Misra DP, Agarwal V, Gasparyan AY, Zimba O (2020) Rheumatologists’ perspective on coronavirus disease 19 (COVID-19) and potential therapeutic targets. Clin Rheumatol 19:2055–2062. https://doi.org/10.1007/s10067-020-05073-9
Benucci M, Damiani A, Infantino M, et al (2020) Médicaments rhumatologiques pour le traitement de l’infection par le COVID-19. Rev du Rhum (Edition Fr 87:150–152 . https://doi.org/10.1016/j.rhum.2020.03.010
Ferro F, Elefante E, Baldini C et al (2020) COVID-19: the new challenge for rheumatologists. Clin Exp Rheumatol:175–180
Graef ER, Liew JW, Putman MS, Simard JF, Sirotich E, Berenbaum F, Duarte-García A, Grainger R, Harrison C, Konig MF, Korsten P, Proulx L, Richards DP, Robinson PC, Sattui SE, Ugarte-Gil MF, Young KJ, Kim AHJ, Sparks JA (2020) Festina lente: hydroxychloroquine, covid-19 and the role of the rheumatologist. Ann Rheum Dis:1–3. https://doi.org/10.1136/annrheumdis-2020-217480
Cron RQ, Chatham WW (2020) The rheumatologist’s role in Covid-19. J Rheumatol. 47:639–642. https://doi.org/10.3899/jrheum.200334
Caricchio R, Criner GJ, Caricchio R (2020) The Journal of Rheumatology Rheumatologists and Pulmonologists at Temple University weather the COVID-19 storm together. 3–5 . https://doi.org/10.3899/jrheum.200740
ACR Suggestions from the American College of Rheumatology for Patients During the COVID-19 Pandemic: How to Navigate Telehealth. In: 2020. https://www.rheumatology.org/Portals/0/Files/Patient-Resources-How-to-Navigate-Telehealth.pdf. Accessed 20 Apr 2020
Putman MS, Ruderman EM (2020) Learning from adversity: lessons from the COVID-19 Crisis. J Rheumatol. 47:791–792. https://doi.org/10.3899/jrheum.200411
Eysenbach G (2012) Improving the quality of web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res:e8. https://doi.org/10.2196/jmir.6.3.e34
Smolen JS, Aletaha D, Bijlsma JWJ, Breedveld FC, Boumpas D, Burmester G, Combe B, Cutolo M, de Wit M, Dougados M, Emery P, Gibofsky A, Gomez-Reino JJ, Haraoui B, Kalden J, Keystone EC, Kvien TK, McInnes I, Martin-Mola E, Montecucco C, Schoels M, van der Heijde D, for the T2T Expert Committee (2010) Treating rheumatoid arthritis to target: recommendations of an international task force. Ann Rheum Dis 69:631–637. https://doi.org/10.1136/ard.2009.123919
UNCTAD (2020) The Coronavirus shock: a story of another global crisis foretold. In: 9 March. https://unctad.org/en/PublicationsLibrary/gds_tdr2019_update_coronavirus.pdf. Accessed 6 Jun 2020
Freites D, Leon L, Mucientes A, et al (2020) Risk factors for hospital admission related to COVID-19 in inflammatory rheumatic diseases. medRxiv 2020.05.14.20101584. https://doi.org/10.1101/2020.05.14.20101584
Government MBRS of (2017) Arab Social Media Report: social media and the internet of things: towards data-driven policymaking in the Arab world. https://www.arabsocialmediareport.com/home/index.aspx. Accessed 30 May 2020
Acknowledgements
The authors would like to thank Professor John Carey and Professor Bassel el Zorkany for critically revising the manuscript.
Author information
Authors and Affiliations
Contributions
NZ, IH, LK designed the study and drafted the questionnaire. All the authors contributed substantially to the work, participated in the recruitment of participants, revised the manuscript critically, approved the submitted version, and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Disclosures
None.
Ethical approval
The study complies with the Declaration of Helsinki. The Ethics Committee of Saint-Joseph University, Beirut, has approved the research protocol (CEHDF 1654).
Consent to participate
All participants gave implicit consent by voluntarily participating in the survey on social media.
Consent for publication
Approved by all authors
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ziadé, N., Hmamouchi, I., el Kibbi, L. et al. The impact of COVID-19 pandemic on rheumatology practice: a cross-sectional multinational study. Clin Rheumatol 39, 3205–3213 (2020). https://doi.org/10.1007/s10067-020-05428-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-05428-2