Abstract
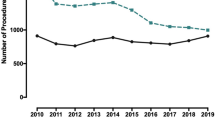
The objective of this study was to assess the time trends in utilization, clinical characteristics, and outcomes of patients undergoing total ankle arthroplasty (TAA) in the USA. We used the Nationwide Inpatient Sample (NIS) data from 1998 to 2010 to examine time trends in the utilization rates of TAA. We used the Cochran Armitage test for trend to assess time trends across the years and the analysis of variance (ANOVA), Wilcoxon test, or chi-squared test (as appropriate) to compare the first (1998–2000) and the last time periods (2009–2010). TAA utilization rate increased significant from 1998 to 2010: 0.13 to 0.84 per 100,000 overall, 0.14 to 0.88 per 100,000 in females, and from 0.11 to 0.81 per 100,000 in males (p < 0.0001 for each comparison for time trends). Compared to the 1998–2000 period, those undergoing TAA in 2009–2010 were older (41 % fewer patients <50 years, p < 0.0001), less likely to have rheumatoid arthritis as the underlying diagnosis (55 % fewer patients, p = 0.0001), more likely to have Deyo-Charlson index of 2 or more (197 % more, p = 0.0010), and had a shorter length of stay at 2.5 days (17 % reduction, p < 0.0001). Mortality was rare ranging from 0 to 0.6 % and discharge to inpatient facility ranged 12.6–14.1 %; we noted no significant time trends in either (p > 0.05). The utilization rate of TAA increased rapidly in the USA from 1998 to 2010, but post-arthroplasty mortality rate was stable. Underlying diagnosis and medical comorbidity changed over time and both can impact outcomes after TAA. Further studies should examine how the outcomes and complications of TAA have evolved over time.

Similar content being viewed by others
References
Maffulli N (2010) Recent advances in foot and ankle surgery: editorial comment. Clin Orthop Relat Res 468(4):921
Park JS, Mroczek KJ (2011) Total ankle arthroplasty. Bull NYU Hosp Jt Dis 69(1):27–35
Coester LM, Saltzman CL, Leupold J, Pontarelli W (2001) Long-term results following ankle arthrodesis for post-traumatic arthritis. J Bone Joint Surg Am 83-A(2):219–228
Anderson T, Montgomery F, Carlsson A (2003) Uncemented STAR total ankle prostheses. Three to eight-year follow-up of fifty-one consecutive ankles. J Bone Joint Surg Am 85-A(7):1321–1329
Knecht SI, Estin M, Callaghan JJ, Zimmerman MB, Alliman KJ, Alvine FG et al (2004) The agility total ankle arthroplasty. Seven to sixteen-year follow-up. J Bone Joint Surg Am 86-A(6):1161–1171
Bai LB, Lee KB, Song EK, Yoon TR, Seon JK (2010) Total ankle arthroplasty outcome comparison for post-traumatic and primary osteoarthritis. Foot Ankle Int 31(12):1048–1056
Conti SF, Wong YS (2001) Complications of total ankle replacement. Clin Orthop Relat Res 391:105–114
Skytta ET, Koivu H, Eskelinen A, Ikavalko M, Paavolainen P, Remes V (2010) Total ankle replacement: a population-based study of 515 cases from the Finnish Arthroplasty Register. Acta Orthop 81(1):114–118
Hosman AH, Mason RB, Hobbs T, Rothwell AG (2007) A New Zealand national joint registry review of 202 total ankle replacements followed for up to 6 years. Acta Orthop 78(5):584–591
Louie GH, Ward MM (2010) Changes in the rates of joint surgery among patients with rheumatoid arthritis in California, 1983–2007. Ann Rheum Dis 69(5):868–871
Kim SH, Wise BL, Zhang Y, Szabo RM (2011) Increasing incidence of shoulder arthroplasty in the United States. J Bone Joint Surg Am 93(24):2249–2254
Kurtz S, Ong K, Lau E, Mowat F, Halpern M (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 89(4):780–785
Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR (2012) Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991–2010. JAMA 308(12):1227–1236
Raikin SM, Rasouli MR, Espandar R, Maltenfort MG (2014) Trends in treatment of advanced ankle arthropathy by total ankle replacement or ankle fusion. Foot Ankle Int 35(3):216–224
Healthcare Cost and Utilization Project. Overview of the Nationwide Inpatient Sample (NIS). http://www.hcup-us.ahrq.gov/nisoverview.jsp Last updated 2/19/13. Rockville, MD: AHRQ; 2012 [6/14/13].
Masoomi H, Mills S, Dolich MO, Ketana N, Carmichael JC, Nguyen NT et al (2012) Comparison of outcomes of laparoscopic versus open appendectomy in children: data from the Nationwide Inpatient Sample (NIS), 2006–2008. World J Surg 36(3):573–578
Shivaraju A, Patel V, Fonarow GC, Xie H, Shroff AR, Vidovich MI (2011) Temporal trends in gastrointestinal bleeding associated with percutaneous coronary intervention: analysis of the 1998–2006 Nationwide Inpatient Sample (NIS) database. Am Heart J 162(6):1062–8 e5
Vassileva CM, Shabosky J, Boley T, Markwell S, Hazelrigg S (2012) Tricuspid valve surgery: the past 10 years from the Nationwide Inpatient Sample (NIS) database. J Thorac Cardiovasc Surg 143(5):1043–1049
Masoomi H, Mills S, Dolich MO, Ketana N, Carmichael JC, Nguyen NT et al (2011) Comparison of outcomes of laparoscopic versus open appendectomy in adults: data from the Nationwide Inpatient Sample (NIS), 2006–2008. J Gastrointest Surg Off J Soc Surg Aliment Tract 15(12):2226–2231
Deyo RA, Cherkin DC, Ciol MA (1992) Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45(6):613–619
Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M (2005) Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am 87(7):1487–1497
Cram P, Lu X, Kaboli PJ, Vaughan-Sarrazin MS, Cai X, Wolf BR et al (2011) Clinical characteristics and outcomes of Medicare patients undergoing total hip arthroplasty, 1991–2008. JAMA 305(15):1560–1567
Jain NB, Higgins LD, Guller U, Pietrobon R, Katz JN (2006) Trends in the epidemiology of total shoulder arthroplasty in the United States from 1990–2000. Arthritis Rheum 55(4):591–597
Jain NB, Higgins LD, Ozumba D, Guller U, Cronin M, Pietrobon R et al (2005) Trends in epidemiology of knee arthroplasty in the United States, 1990–2000. Arthritis Rheum 52(12):3928–3933
Jain N, Pietrobon R, Hocker S, Guller U, Shankar A, Higgins LD (2004) The relationship between surgeon and hospital volume and outcomes for shoulder arthroplasty. J Bone Joint Surg Am 86-A(3):496–505
Katz JN, Losina E, Barrett J, Phillips CB, Mahomed NN, Lew RA et al (2001) Association between hospital and surgeon procedure volume and outcomes of total hip replacement in the United States medicare population. J Bone Joint Surg Am 83-A(11):1622–1629
Acknowledgments
JAS is supported by grants from the Agency for Health Quality and Research Center for Education and Research on Therapeutics (AHRQ CERTs) U19 HS021110; the National Institute of Arthritis, Musculoskeletal and Skin Diseases (NIAMS) P50 AR060772 and U34 AR062891; the National Institute of Aging (NIA) U01 AG018947; the National Cancer Institute (NCI) U10 CA149950; and research contract CE-1304-6631 from Patient Centered Outcomes Research Institute (PCORI). JAS is also supported through the use of resources and facilities at the VA Medical Center at Birmingham, AL, USA.
Disclosures
There are no financial conflicts related directly to this study. JAS has received research and travel grants from Takeda and Savient and consultant fees from Savient, Takeda, Ardea, and Regeneron. RR has no conflicts.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Singh, J.A., Ramachandran, R. Time trends in total ankle arthroplasty in the USA: a study of the National Inpatient Sample. Clin Rheumatol 35, 239–245 (2016). https://doi.org/10.1007/s10067-014-2703-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-014-2703-2