Abstract
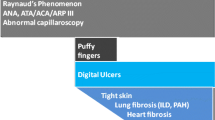
This study aims to analyze differences among established disease damage indicators in patients with limited cutaneous systemic sclerosis (lcSSc) and diffuse cutaneous systemic sclerosis (dcSSc). Fifty patients with lcSSc and 55 patients with dcSSc were included in this study. Difference in mean disease duration between the two subgroups of patients was not statistically significant (z=−0.88, p=0.38). Patients with lcSSc and dcSSc were compared, and differences in vascular, esophageal, lung, heart, renal, and musculoskeletal involvement were statistically assessed using χ 2, Mann–Whitney, and Kruskal–Wallis tests. Using the technique of nailfold capillaroscopy, we found normal capillaries or nonspecific capillary change in 10.0% of the patients with lcSSc and only in 3.6% of the patients with dcSSc. Dilated capillaries without loss of capillaries were found in 42% of the patients with lcSSc and in 10.9% of the patients with dcSSc (p=0.05). However, severe capillary damage (loss of capillaries) was noticed more frequently in patients with dcSSc (dcSSc/lcSSc: 85.5%/48.0%, p=0.002). Pitting scars or digital ulcers were found in 46.0% of the patients with lcSSc and in 67.3% of the patients with dcSSc (p=0.04). We did not notice a significant difference in frequency of fingertip osteolysis and telangiectasia. Esophageal hypomotility was found in 64% of the patients with lcSSc and in 85.5% of the patients with dcSSc (p<0.01). We found interstitial lung fibrosis more frequently in patients with dcSSc (lcSSc/dcSSc: 16.0%/72.7%, p<0.001). Reduced forced vital capacity (FVC) was found in 6.0% of the of patients with lcSSc and in 41.8% of the patients with dcSSc (p<0.001). A decreased value of the transfer factor for carbon monoxide (DLCO) was also observed more frequently in patients with dcSSc. Heart involvement was found in 29.1% of the patients with dcSSc and less frequently (p<0.001) in patients with lcSSc (8%). Similarly, we found renal involvement more frequently in patients with dcSSc (lcSSc/dcSSc: 2.0%/16.3%). Tendon friction rubs were noticed in 23.6% of the patients with dcSSc and only in 6% of the patients with lcSSc (p<0.01). Joint contractures were observed in 70.9% of the patients with dcSSc and in 26.0% of the patients with lcSSc (p<0.001). Muscle weakness was noticed more frequently in patients with dcSSc (lcSSc/dcSSc: 22.0%/40.0%, p<0.05). Arthralgia was found more frequently in patients with dcSSc, but arthritis became apparent, without significant difference in frequency, in 16% of the patients with lcSSc and in 16.4% of the patients with dcSSc. Loss of capillaries (detected by nailfold capillaroscopy), digital ulcers, interstitial lung fibrosis, decreased FVC and DLCO, esophageal hypomotility, musculoskeletal impairment, and heart and renal involvement are more common in patients with dcSSc. Fingertip osteolysis, telangiectasia, and arthritis are equally frequent in both forms of the disease.
Similar content being viewed by others
References
Seibold JR (1997) Scleroderma. In: Kelley WN, Harris ED, Ruddy S, Sledge CB (eds) Textbook of rheumatology, 5th edn. Saunders, Philadelphia, pp 1133–1163
Cervini C, Grassi W (1996) Raynaud's phenomenon. Rheumatol Eur 25(3):111–113
Kahleh MB, Suttany GL, Smith EA et al (1986) A modified scleroderma skin scoring method. Clin Exp Rheumatol 14:367–369
Behr J, Vogelmeier C, Beinert T et al (1996) Bronchoalveolar lavage for evaluation and management of scleroderma disease of the lung. Clin Exp Rheumatol 154:400–406
Preston IR, Hill NS (2003) Evaluation and management of pulmonary hypertension in systemic sclerosis. Curr Opin Rheumatol 15(6):761–765
Seibold JR (1993) Scleroderma. In: Kelley WN (ed) Arthritis and allied conditions. Saunders, Philadelphia, pp 1113–1143
Subcommittee for Scleroderma Criteria of the American Rheumatism Association Diagnostic and Therapeutic Criteria Committee (1980) Preliminary criteria for the classification of systemic sclerosis (scleroderma). Arthritis Rheum 23:581–590
Le Roy EC, Black C, Fleischmajer et al (1988) Scleroderma (systemic sclerosis): classification, subsets and pathogenesis. J Rheumatol 15:202–205
Giordano M, Valentini G, Migliaresi S et al (1986) Different antibody patterns and different prognoses in patients with scleroderma with various extent of skin sclerosis. J Rheumatol 13:202–205
Damjanov N (1995) Significance of capillaroscopic findings for the diagnosis of systemic sclerosis. Acta Rheumatol Belgrad 15(1):61–86
Jacobsen S, Halberg P, Ullman S et al (1998) Clinical features and serum antinuclear antibodies in 230 Danish patients with systemic sclerosis. J Rheumatol 37:39–45
Steen VD, Powell DL, Medsger TA Jr (1988) Clinical correlations and prognosis based on serum autoantibodies in patients with systemic sclerosis. Arthritis Rheum 31:196–203
Satoh M, Akizuki M, Kuwana M et al (1994) Genetic and immunological differences between Japanese patients with diffuse scleroderma and limited scleroderma. J Rheumatol 21:111–114
Harris M, Rosen A (2003) Autoimmunity on scleroderma: the origin, pathogenetic role, and clinical significance of autoantiodies. Curr Opin Rheumatol 15:778–784
Morelli S, Barbieri C, Sgreccia A et al (1997) Relationship between cutaneous and pulmonary involvement in systemic sclerosis. J Rheumatol 24:81–85
Kane GC, Varga J, Conant EF et al (1996) Lung involvement in systemic sclerosis (scleroderma): relation to classification based on extent of skin involvement and autoantibody status. Respir Med 90:223–230
Diot E, Giraudeau B, Diot P et al (1999) Is anti-topoisomerase I a serum marker of pulmonary involvement in systemic sclerosis? Chest 116:715–720
Steen V, Medsger T (2000) Severe organ involvement in patient with diffuse scleroderma. Arthritis Rheum 43:2437–2444
Denton C (2003) Renal complications of systemic sclerosis. Ann Rheum Dis 62(Suppl 1):SP0014
Della Rosa A, Valentini G, Bombardieri A et al (2001) European multicentre study to define disease activity criteria for systemic sclerosis. Clinical and epidemiological features of 290 patients from 19 centers. Ann Rheum Dis 60:585–591
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ostojić, P., Damjanov, N. Different clinical features in patients with limited and diffuse cutaneous systemic sclerosis. Clin Rheumatol 25, 453–457 (2006). https://doi.org/10.1007/s10067-005-0041-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-005-0041-0