Abstract
Pulmonary artery hypertension (PAH) remains the leading cause of morbidity and mortality in systemic sclerosis, while Raynaud’s phenomenon and digital ulcers significantly add to the morbidity in systemic sclerosis (SSc). This study was undertaken to evaluate the role of sildenafil in PAH, Raynaud’s phenomenon, and digital ulcers in systemic sclerosis patients. A prospective, open-label, uncontrolled pilot study was done at a tertiary care centre in India to study the safety and efficacy of oral sildenafil in PAH, Raynaud’s phenomenon, digital infarcts, and ulcers in SSc. Seventeen patients fulfilling ACR classification criteria for scleroderma and having PAH were recruited. Six-minute walk test, WHO class of dyspnoea, severity of Raynaud’s phenomenon, and 2D ECHO were performed in all the study subjects at baseline and at 3 months post-treatment. All patients were treated with oral sildenafil 25 mg three times a day for a period of 3 months. The pre- and post-treatment values of mean pulmonary artery pressure (PAP), 6-min walk test, WHO class of dyspnoea, and severity of Raynaud’s phenomenon were compared to look for any significant change. Sixteen patients who completed 3-month follow-up had shown statistically significant improvement in 6-min walk test, WHO class of dyspnoea, severity of Raynaud’s phenomenon, and mPAP. Also, there was no occurrence of new digital infarcts or ulcers, and existing ulcers showed signs of healing. Sildenafil is highly efficacious cheaper and safe alternative to other available therapies for SSc-associated PAH, Raynaud’s phenomenon, and digital infarcts/ulcers.
Similar content being viewed by others
Introduction
Systemic sclerosis (SSc) is a chronic multisystem disorder of unknown aetiology, characterized by fibrosis, vasculopathy, and altered immune status [1].
Pulmonary artery hypertension (PAH) occurs in 16–33 % of the patients with SSc and accounts for about 25 % of all causes of death in SSc [2, 3].
It can be (1) primary—isolated PAH—and (2) secondary—due to interstitial lung disease. SSc patients with PAH are at higher risk of death than patients with idiopathic PAH, despite similar haemodynamic patterns and treatments, with respective estimated 1-year survival rates of 55–84 % [4].
Available vasodilator therapies like calcium antagonist, prostacyclin analogues, and endothelin receptor antagonist are found to have limited success due to non-selectivity, cost, availability, adverse effects, and potential complications.
In the search for alternative therapeutic targets in PAH, cyclic guanosine monophosphate–dependent phosphodiesterase type-5 has emerged as an attractive option. There are few studies demonstrating efficacy of sildenafil in PAH in scleroderma [5–11].
Sildenafil improves exercise capacity and quality of life in patients with systolic heart failure and secondary pulmonary hypertension. Also, there is some evidence that sildenafil has beneficial effect on Raynaud’s phenomenon and digital infarcts in scleroderma [12].
With this background knowledge, this work was done to study the safety and efficacy of sildenafil in SSc patients with PAH.
Materials and methods
It is a prospective, open-label, uncontrolled pilot study conducted at a tertiary care centre in India. Seventeen patients were recruited from Medicine OPD, Medicine wards & Rheumatology clinic. Institute Human Ethics Committee approved the protocol.
Inclusion criteria
(1) All patients of scleroderma fulfilling ACR classification criteria having PAH; (2) age more than 18 years; and (3) the patient giving written consent to participate in the study.
Exclusion criteria
(1) Overlap syndrome, (2) patients having hepatic disease or failure (ALT or AST 5 × upper limit of normal or jaundice), (3) patients having renal disease or failure (requires dialysis or a creatinine ≥1.4 mg/dl), (4) patients concurrently or intermittently using organic nitrates in any form, and (5) pregnant or lactating women
Detailed history and examination was done. Severity of Raynaud’s phenomenon was graded as per Gemne’s classification [13].
Patients were subjected to baseline laboratory investigations including complete haemogram, liver function test, renal function test, urine routine and microscopy, ECG, chest skiagram, and antinuclear antibody (ANA). Pulmonary function test (PFT), high-resolution computerized tomogram (HRCT) chest, and 6-min walk test were performed in all the study subjects. All the recruited patients were treated with oral sildenafil 25 mg three times a day for a period of 3 months. Clinical parameters like 6-min walk test, WHO class of dyspnoea, and severity of Raynaud’s phenomenon were compared with the pre-treatment values. All the patients underwent repeat 2D ECHO after 3 months to measure mean PAP. The pre- and post-treatment values of mean PAP were compared to look for any significant change.
Echocardiographic principle
Pulmonary arterial hypertension alters the timing of pulmonary valve opening and closure pattern, pulmonary valve motion, and the shape of pulmonary blood flow velocity profile.
When pulmonary hypertension is present, pulmonary artery end-diastolic pressure exceeds right ventricular pressure reducing or eliminating any effect of atrial contraction on pulmonary valve motion. As pulmonary artery pressure increases, the time required for the right ventricular pressure to rise to the level of end-diastolic pulmonary pressure will increase and the valve will open later than normal. The rate of rise of right ventricular pressure (dp/dt) at the time of valve opening is generally greater than that of normal with the result that valve opening and flow acceleration are more rapid. Pulmonary valve closure occurs slightly earlier than normal, and the time for right ventricular pressure to fall to the level of right atrial pressure increases.
The other approach will be to measure the pulmonary artery systolic pressure from right ventricular systolic pressure (assuming no pulmonary stenosis) determined as sum of transtricuspid gradient and either as assumed or as clinically determined right atrial pressure.
Technique
Patients were evaluated in supine and left lateral position by a trained, experienced cardiologist. An ECG was taken with simultaneous strip chart recording at speed 50 and 100 mm/sec. A non-imaging continuous wave Doppler signal with Doptek at 3.5/2.7 MHz transducer was used for doing echocardiography. A systematic search was made using two-dimensional and colour flow Doppler to identify tricuspid regurgitation jet followed by continuous wave. The peak instantaneous drop in systolic pressure from right ventricle to atrium was calculated from the peak of signal velocity of the tricuspid regurgitant signal by a simplified Bernoulli’s equation. Dp = 4V2 where Dp is the trans-tricuspid gradient and V is the peak velocity measured. Final estimate of the pulmonary artery systolic pressure was obtained by adding the patient jugular venous pressure to the estimate of the trans-tricuspid gradient. The right ventricular systolic time intervals were recorded under three headings:
-
1.
Acceleration time (ACT),
-
2.
Acceleration time index (ATI),
-
3.
Tricuspid gradient.
Flow profile across the pulmonary valve is also considered. Patient was considered having pulmonary hypertension if they fulfilled either of the two criteria:
-
1.
Tricuspid gradient more than 35 mm Hg
(Or)
-
2.
Right ventricular acceleration time of less than 90 ms
Mean PA pressure is derived from right ventricular acceleration time (RVAT) by the following formula: 78−0.45 × RVAT, where RVAT is in milliseconds.
Results
Out of 74 patients of SSc screened for PAH, 17 patients fulfilling inclusion criteria were recruited for the study. Out of 17 patients, only 16 patients completed 3-month follow-up. Baseline characteristics of patients are given in Table 1.
All the patients had dyspnoea at presentation. The dyspnoea was classified according to WHO functional classification and graded as class I to class IV. Six patients (37 %) had dyspnoea class II, whereas 10 patients (63 %) had dyspnoea class III.
All the patients had Raynaud’s phenomenon that was categorized as mild, moderate, and severe according to Gemne’s classification. Ten patients (63 %) had severe, 4 subjects (25 %) had moderate, whereas 2 subjects (12 %) had mild symptoms.
All the patients in the study had interstitial lung disease, which was diagnosed on the basis of high-resolution CT scan of the chest and pulmonary function tests.
Pre- and post-treatment analysis
Mean pulmonary artery pressure decreased from 44.5 ± 5.3 mm Hg to 27.2 ± 8.3 mm Hg at the end of 3 months with average reduction of 18.3 mm Hg. The observed reduction was statistically significant with p value less than 0.001.
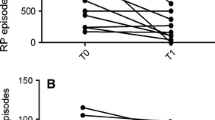
The 6-min walk distance increased from 296.1 ± 48.9 m to 415.6 ± 47.8 m with average increase of 119.5 m (p < 0.001) as shown in Fig. 1. Similarly, WHO functional class of patients showed a significant improvement at the end of 3 months as assessed by Wilcoxon signed rank test with p value 0.04 as shown in Fig. 2. There was statistically significant improvement in frequency and severity of Raynaud’s phenomenon in the patients at the end of 3 months when analysed by Wilcoxon signed rank test as shown in Fig. 3. Three out of these 7 patients (43 %) noted complete healing of digital ulcers, whereas remaining 4 patients (57 %) noted significant improvement in the ulcers. None of the subjects noted appearance of new ulcers during the course of therapy with sildenafil.
Side effects of the drug
Five out of 16 patients (32 %) reported headache, which was pronounced at the start of therapy. The headache was either self-resolving or it responded to oral paracetamol. None of the patients complained of rash, visual disturbances, sneezing, flushing, dyspepsia, or palpitations. None of the patients had deranged haemogram and biochemical tests at 3 months.
Discussion
The decrease in mean PAP observed in our study is comparable to or better than that reported in the literature. Sastry et al. [14] studied 29 patients with primary PPH. The average systolic PAP decreased by 14 mmHg (from 109.26 mm Hg to 95.15 post-treatment, p < 0.008) at the end of 3 months with sildenafil therapy from 75 mg per day to 300 mg per day as tolerated [14]. Galie et al. [6] studied a total of 278 patients with PAH—both primary and secondary. The average decrease in mean pulmonary artery pressure at the end of 12 weeks was between 2.1 mm Hg and 4 mm Hg in patients receiving sildenafil (p < 0.001) [6]. Similarly in a randomized, double-blind, placebo-controlled crossover study of twenty patients with PAH, both primary and secondary pulmonary artery pressure improved from the baseline of 98.8 ± 20.5 mm Hg to 78.3 ± 15.3 mm Hg (p < 0.0001) at the end of 3 months on treatment with sildenafil [15]. Garg et al. [16] evaluated the efficacy of oral sildenafil in 44 patients of severe PAH. On follow-up cardiac catheterization, after 10 weeks of sildenafil treatment (150 mg per day), a significant reduction in mean pulmonary arterial pressure (from 67.0 ± 10.2 to 56.9 ± 9.5 mm Hg, p = 0.001) was noted [16].
Kuang et al. [17] carried out extensive meta-analysis to review the role of sildenafil in the treatment for PAH, which showed that compared with placebo treatment, sildenafil therapy decreases the pulmonary artery systolic pressure by 11.51 mmHg on an average (p = 0.03) in patients with PAH at the end of average of 12 weeks of therapy in average dose of 100 mg per day [17].
Six-minute walk test
Six-minute walk test is an excellent clinical test to evaluate cardiopulmonary status. It indirectly correlates positively with the severity of pulmonary artery hypertension. Among non-invasive parameters including clinical, echocardiographic, and neurohumoral parameters, only the distance walked in 6 min was independently related to mortality in PPH by multivariate analysis [18].
We observed a significant improvement in the distance from 296.1 ± 48.9 m to 415.6 ± 47.8 m with average increase of 119.5 m (p < 0.001). The significant improvement in 6-min walk test observed in the study has several important implications. First, it indicates improvement in walking distance and functional class of patients with scleroderma, which points towards significant improvement in quality of life. Next, it points towards beneficial effects of sildenafil on pulmonary haemodynamics and cardiopulmonary status of the patients receiving this drug. Similar results have been obtained in the other studies, and the improvement in the 6-min walk test distance has been strongly correlated with improvement in mean pulmonary artery pressure measured by 2 D ECHO and cardiac catheterization studies.
In the study carried out by Galie et al. [6] in 278 patients of PAH with 39 patients of scleroderma, in subgroup analysis, they noticed average increase of 50 m in 6-min walk test from 396 ± 42 m to 446 ± 47 m (p < 0.05) [6].
Badesch et al. [9] studied that 84 patients with PAH with connective tissue disease were treated with sildenafil 20 mg tds to 80 mg tds; 45 % of the patients had scleroderma. Sildenafil-treated patients exhibited mean increases in 6-minute walk distance at week 12 by 42 m for 20 mg, 36 m for 40 mg, and 15 m for 80 mg, while placebo-treated patients exhibited a mean decrease of 13 m (p < 0.05) [9].
WHO functional class
We observed a significant improvement in WHO functional class of patients. Twelve out of 16 patients (80 %) noted improvement in WHO functional class, and the remaining 4 patients noted no benefit; however, none of the patients deteriorated. Similar results have been shown by other studies [6, 14]. The improvement in WHO functional class can be attributed to improvement in mean PAP and 6-min walk test distance.
Raynaud’s phenomenon
We observed decrease in both frequency and severity of Raynaud’s phenomenon. Eighty percentage of our patients showed statistically significant improvement (p < 0.05), and none had deteriorated. The beneficial effect of sildenafil on Raynaud’s phenomenon could be attributed to the vasodilator effect. Similar findings were noted in the study conducted by Fries et al. in 16 patients with Raynaud’s phenomenon where the mean capillary flow velocity of all patients more than quadrupled after treatment with sildenafil (0.53 mm/s versus 0.13 mm/s, p = 0.0004) [19].
In the extensive data analysis done by Levien from 1996 to 2006 of all available studies regarding use of sildenafil in Raynaud’s phenomenon, it was concluded that the drug reduces frequency, duration, as well as severity of Raynaud’s symptoms in both primary and secondary Raynaud’s phenomenon [17].
Digital ulcers
There was a significant improvement in digital ulcers in these patients at the end of 3 months. Most of the patients noted improvement in the digital ulcers, and 3 out of 16 patients reported complete healing of the ulcers. There were no new digital ulcers during 3 months of therapy with sildenafil.
Sildenafil has also shown benefit in healing of acral ulcers in patients with scleroderma [20]. The literature is limited, but the results reported are quite impressive.
Side effects of the drug
Five out of 16 patients complained of headache, which was either self-resolving as in 2 patients or responded to oral paracetamol. We did not observe any serious side effects like rash, hepatic or renal dysfunction, visual disturbances, and bleeding manifestations. Our results are comparable to majority of studies, and the drug appears to be safe in prescribed doses [21–23].
Majority of studies have studied sildenafil in primary pulmonary hypertension, but the data on the effect of sildenafil on scleroderma-associated PAH are limited. Sildenafil gives a cheap yet highly effective treatment for PAH in scleroderma especially in resource constraint setting. The additional benefit it offers in Raynaud’s phenomenon helps in improving the quality of life of patients with scleroderma. The main drawbacks of our study were the following: (1) it was an observational study without any control arm; (2) invasively measured haemodynamic data through cardiac catheterization before and after sildenafil therapy for the whole group would have been ideal; and (3) long-term benefit of drug cannot be deducted from this study, and also dose-dependent effect on mean pulmonary artery pressure cannot be studied.
In spite of these limitations, our data support the use of sildenafil in patients with scleroderma-associated PAH and Raynaud’s phenomenon. But, whether the reduction in mean pulmonary artery pressure translates into mortality benefit needs to be studied.
References
Denton CP, Black CM, Abraham DJ (2009) Mechanism and consequence of fibrosis in systemic sclerosis. Nat Clin Pract Rheumatol 2:134–144
Trad S, Amoura Z, Beigelman C et al (2006) Pulmonary arterial hypertension is a major mortality factor in diffuse systemic sclerosis independent of interstitial lung disease. Arthritis Rheum 54(1):184–191
Magliano M, Isenberg DA, Hillson J (2002) Pulmonary hypertension in autoimmune rheumatic diseases: where are we now? Arthritis Rheum 46(8):1997–2009
Kawut SM, Taichman DB, Archer-Chicko CL (2003) Hemodynamics and survival in patients with pulmonary arterial hypertension related to systemic sclerosis. Chest 123:344–350
Watanabe H, Ohashi K, Takeuchi K et al (2002) Sildenafil for primary and secondary pulmonary hypertension. Clin Pharmacol Ther 71(5):398–402
Galiè N, Ghofrani HA, Torbicki A et al (2005) Sildenafil use in pulmonary arterial hypertension (SUPER) Study Group. Sildenafil citrate therapy for pulmonary arterial hypertension. N Engl J Med 353(20):2148–2157
Wilkins MR, Paul GA, Strange JW et al (2005) Sildenafil versus endothelin receptor antagonist for pulmonary hypertension (SERAPH) study. Am J Respir Crit Care Med 171(11):1292–1297
Lewis GD, Shah R, Shahzad K et al (2007) Sildenafil improves exercise capacity and quality of life in patients with systolic heart failure and secondary pulmonary hypertension. Circulation 116(14):1555–1562
Badesch DB, Hill NS, Burgess G, SUPER Study Group et al (2007) Sildenafil for pulmonary arterial hypertension associated with connective tissue disease. J Rheumatol 34(12):2417–2422
Xu XQ, Jing ZC, Zhang JH et al (2009) The efficacy and safety of sildenafil in Chinese patients with pulmonary arterial hypertension. Hypertens Res 32(10):911–915
Samarzija M, ZuljeviÄ E, JakopoviÄ M et al (2009) One year efficacy and safety of oral sildenafil treatment in severe pulmonary hypertension. Coll Antropol 33(3):799–803
Levien TL (2006) Phosphodiesterase inhibitors in Raynaud’s phenomenon. Ann Pharmacother 40(7–8):1388–1393
Gemne G (1997) Diagnostics of hand-arm system disorders in workers who use vibrating tools. Occup Environ Med 54(2):90–95
Sastry BK, Narasimhan C, Reddy NK et al (2002) Study of clinical efficacy of sildenafil in patients with primary pulmonary hypertension. Indian Heart J 54:410–414
Singh TP, Rohit M, Grover A (2006) A randomized, placebo-controlled, double-blind, crossover study to evaluate the efficacy of oral sildenafil therapy in severe pulmonary artery hypertension. Am Heart J 151(4):851–855
Garg N, Sharma MK, Sinha N (2007) Role of oral sildenafil in severe pulmonary arterial hypertension: clinical efficacy and dose response relationship. Int J Cardiol 120(3):306–313
Kuang TG, Wang J, Zhai ZG (2007) Efficacy and safety of sildenafil therapy in pulmonary artery hypertension: a meta-analysis. Zhonghua Yi Xue Za Zhi 87(15):1021–1024
Miyamoto S, Nagaya N, Satoh T et al (2000) Clinical correlates and prognostic significance of six minutes’ walk test in patients with primary pulmonary hypertension. Am J Respir Crit Care Med 161:487–492
Fries R, Shariat K, von Wilmowsky H et al (2005) Sildenafil in the treatment of Raynaud's phenomenon resistant to vasodilatory therapy. Circulation 112:2980–2985
Friedrichson E, Rehberger P, Fuhrmann JT et al (2008) Fast and efficient healing of scleroderma-associated acral ulcers with sildenafil. Hautarzt 59(3):230–232
Jackson G, Benjamin N, Jackson N et al (1999) Effect of sildenafil citrate on human hemodynamics. Am J Cardiol 83(5A):13C–20C
Watanabe H, Ohashi K, Takeuchi K et al (2002) Sildenafil for primary and secondary pulmonary hypertension. Clin Pharmacol Ther 71:398–402
Rosenkranz S, Diet F, Karasch T et al (2003) Sildenafil improved pulmonary hypertension and peripheral blood flow in a patient with scleroderma-associated lung fibrosis and the raynaud phenomenon. Ann Intern Med 134(10):871–872
Acknowledgments
None.
Conflict of interest
None.
Ethics approval
Ethics approval was taken from Institute Human Ethics Committee.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kumar, U., Gokhle, S.S., Sreenivas, V. et al. Prospective, open-label, uncontrolled pilot study to study safety and efficacy of sildenafil in systemic sclerosis–related pulmonary artery hypertension and cutaneous vascular complications. Rheumatol Int 33, 1047–1052 (2013). https://doi.org/10.1007/s00296-012-2466-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-012-2466-5