Abstract
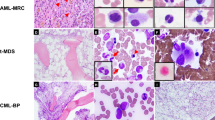
Myelodysplasia (MDS) and acute myeloid leukemia (AML) are heterogeneous, closely associated diseases arising de novo or following chemotherapy with alkylating agents, topoisomerase II inhibitors, or after radiotherapy. Whereas de novo MDS and AML are almost always subclassified according to cytogenetic characteristics, therapy-related MDS (t-MDS) and therapy-related AML (t-AML) are often considered as separate entities and are not subdivided. Alternative genetic pathways were previously proposed in t-MDS and t-AML based on cytogenetic characteristics. An increasing number of gene mutations are now observed to cluster differently in these pathways with an identical pattern in de novo and in t-MDS and t-AML. An association is observed between activating mutations of genes in the tyrosine kinase RAS–BRAF signal-transduction pathway (Class I mutations) and inactivating mutations of genes encoding hematopoietic transcription factors (Class II mutations). Point mutations of AML1 and RAS seem to cooperate and predispose to progression from t-MDS to t-AML. Recently, critical genetic effects underlying 5q−/−5 and 7q−/−7 have been proposed. Their association and cooperation with point mutations of p53 and AML1, respectively, extend the scenario of cooperating genetic abnormalities in MDS and AML. As de novo and t-MDS and t-AML are biologically identical diseases, they ought to be subclassified and treated similarly.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Grimwade D, Walker H, Oliver F, Wheatley K, Harrison C, Harrison G et al. The importance of diagnostic cytogenetics on outcome in AML: analysis of 1612 patients entered into the MRC AML 10 trial. The Medical Research Council Adult and Children's Leukaemia Working Parties. Blood 1998; 92: 2322–2333.
Slovak ML, Kopecky KJ, Cassileth PA, Harrington DH, Theil KS, Mohamed A et al. Karyotypic analysis predicts outcome of preremission and postremission therapy in adult acute myeloid leukemia: a Southwest Oncology Group/Eastern Cooperative Oncology Group Study. Blood 2000; 96: 4075–4083.
Byrd JC, Mrozek K, Dodge RK, Carroll AJ, Edwards CG, Arthur DC et al. Pretreatment cytogenetic abnormalities are predictive of induction success, cumulative incidence of relapse, and overall survival in adult patients with de novo acute myeloid leukemia: results from Cancer and Leukemia Group B (CALGB 8461). Blood 2002; 100: 4325–4336.
Sanderson RN, Johnson PR, Moorman AV, Roman E, Willett E, Taylor PR et al. Population-based demographic study of karyotypes in 1709 patients with adult acute myeloid leukemia. Leukemia 2006; 20: 444–450.
Greenberg P, Cox C, LeBeau MM, Fenaux P, Morel P, Sanz G et al. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood 1997; 89: 2079–2088.
Look AT . Oncogenic transcription factors in the human acute leukemias. Science 1997; 278: 1059–1064.
Zhang Y, Rowley JD . Chromatin structural elements and chromosomal translocations in leukemia. DNA Repair (Amst) 2006; 5: 1282–1297.
Pedersen-Bjergaard J, Andersen MK, Christiansen DH, Nerlov C . Genetic pathways in therapy-related myelodysplasia and acute myeloid leukemia. Blood 2002; 99: 1909–1912.
Nakano Y, Kiyoi H, Miyawaki S, Asou N, Ohno R, Saito H et al. Molecular evolution of acute myeloid leukaemia in relapse: unstable N-ras and FLT3 genes compared with p53 gene. Br J Haematol 1999; 104: 659–664.
Kottaridis PD, Gale RE, Frew ME, Harrison G, Langabeer SE, Belton AA et al. The presence of a FLT3 internal tandem duplication in patients with acute myeloid leukemia (AML) adds important prognostic information to cytogenetic risk group and response to the first cycle of chemotherapy: analysis of 854 patients from the United Kingdom Medical Research Council AML 10 and 12 trials. Blood 2001; 98: 1752–1759.
Stirewalt DL, Kopecky KJ, Meshinchi S, Appelbaum FR, Slovak ML, Willman CL et al. FLT3, RAS, and TP53 mutations in elderly patients with acute myeloid leukemia. Blood 2001; 97: 3589–3595.
Thiede C, Steudel C, Mohr B, Schaich M, Schakel U, Platzbecker U et al. Analysis of FLT3-activating mutations in 979 patients with acute myelogenous leukemia: association with FAB subtypes and identification of subgroups with poor prognosis. Blood 2002; 99: 4326–4335.
Schnittger S, Schoch C, Dugas M, Kern W, Staib P, Wuchter C et al. Analysis of FLT3 length mutations in 1003 patients with acute myeloid leukemia: correlation to cytogenetics, FAB subtype, and prognosis in the AMLCG study and usefulness as a marker for the detection of minimal residual disease. Blood 2002; 100: 59–66.
Care RS, Valk PJ, Goodeve AC, Abu-Duhier FM, Geertsma-Kleinekoort WM, Wilson GA et al. Incidence and prognosis of c-KIT and FLT3 mutations in core binding factor (CBF) acute myeloid leukaemias. Br J Haematol 2003; 121: 775–777.
Preudhomme C, Sagot C, Boissel N, Cayuela JM, Tigaud I, De Botton S et al. Favorable prognostic significance of CEBPA mutations in patients with de novo acute myeloid leukemia: a study from the Acute Leukemia French Association (ALFA). Blood 2002; 100: 2717–2723.
Gombart AF, Hofmann WK, Kawano S, Takeuchi S, Krug U, Kwok SH et al. Mutations in the gene encoding the transcription factor CCAAT/enhancer binding protein alpha in myelodysplastic syndromes and acute myeloid leukemias. Blood 2002; 99: 1332–1340.
Frohling S, Schlenk RF, Stolze I, Bihlmayr J, Benner A, Kreitmeier S et al. CEBPA mutations in younger adults with acute myeloid leukemia and normal cytogenetics: prognostic relevance and analysis of cooperating mutations. J Clin Oncol 2004; 22: 624–633.
Falini B, Mecucci C, Tiacci E, Alcalay M, Rosati R, Pasqualucci L et al. Cytoplasmic nucleophosmin in acute myelogenous leukemia with a normal karyotype. N Engl J Med 2005; 352: 254–266.
Verhaak RG, Goudswaard CS, van Putten W, Bijl MA, Sanders MA, Hugens W et al. Mutations in nucleophosmin (NPM1) in acute myeloid leukemia (AML): association with other gene abnormalities and previously established gene expression signatures and their favorable prognostic significance. Blood 2005; 106: 3747–3754.
Dohner K, Schlenk RF, Habdank M, Scholl C, Rucker FG, Corbacioglu A et al. Mutant nucleophosmin (NPM1) predicts favorable prognosis in younger adults with acute myeloid leukemia and normal cytogenetics: interaction with other gene mutations. Blood 2005; 106: 3740–3746.
Suzuki T, Kiyoi H, Ozeki K, Tomita A, Yamaji S, Suzuki R et al. Clinical characteristics and prognostic implications of NPM1 mutations in acute myeloid leukemia. Blood 2005; 106: 2854–2861.
Thiede C, Koch S, Creutzig E, Steudel C, Illmer T, Schaich M et al. Prevalence and prognostic impact of NPM1 mutations in 1485 adult patients with acute myeloid leukemia (AML). Blood 2006; 107: 4011–4020.
Pasqualucci L, Liso A, Martelli MP, Bolli N, Pacini R, Tabarrini A et al. Mutated nucleophosmin detects clonal multilineage involvement in acute myeloid leukemia: Impact on WHO classification. Blood 2006; 108: 4146–4155.
Deguchi K, Gilliland DG . Cooperativity between mutations in tyrosine kinases and in hematopoietic transcription factors in AML. Leukemia 2002; 16: 740–744.
Kelly LM, Gilliland DG . Genetics of myeloid leukemias. Annu Rev Genomics Hum Genet 2002; 3: 179–198.
Rowley JD, Golomb HM, Vardiman JW . Nonrandom chromosome abnormalities in acute leukemia and dysmyelopoietic syndromes in patients with previously treated malignant disease. Blood 1981; 58: 759–767.
Pedersen-Bjergaard J, Rowley JD . The balanced and the unbalanced chromosome aberrations of acute myeloid leukemia may develop in different ways and may contribute differently to malignant transformation. Blood 1994; 83: 2780–2786.
Pedersen-Bjergaard J, Andersen MK, Johansson B . Balanced chromosome aberrations in leukemias following chemotherapy with DNA-topoisomerase II inhibitors. J Clin Oncol 1998; 16: 1897–1898.
Christiansen DH, Andersen MK, Pedersen-Bjergaard J . Mutations with loss of heterozygosity of p53 are common in therapy-related myelodysplasia and acute myeloid leukemia after exposure to alkylating agents and significantly associated with deletion or loss of 5q, a complex karyotype, and a poor prognosis. J Clin Oncol 2001; 19: 1405–1413.
Christiansen DH, Pedersen-Bjergaard J . Internal tandem duplications of the FLT3 and MLL genes are mainly observed in atypical cases of therapy-related acute myeloid leukemia with a normal karyotype and are unrelated to type of previous therapy. Leukemia 2001; 15: 1848–1851.
Christiansen DH, Andersen MK, Pedersen-Bjergaard J . Mutations of AML1 are common in therapy-related myelodysplasia following therapy with alkylating agents and are significantly associated with deletion or loss of chromosome arm 7q and with subsequent leukemic transformation. Blood 2004; 104: 1474–1481.
Christiansen DH, Andersen MK, Desta F, Pedersen-Bjergaard J . Mutations of genes in the receptor tyrosine kinase (RTK)/RAS-BRAF signal transduction pathway in therapy-related myelodysplasia and acute myeloid leukemia. Leukemia 2005; 19: 2232–2240.
Desta F, Christiansen DH, Andersen MK, Pedersen-Bjergaard J . Activating mutations of JAK2V617F are uncommon in t-MDS and t-AML and are only observed in atypic cases. Leukemia 2006; 20: 547–548.
Christiansen DH, Desta F, Andersen MK, Pedersen-Bjergaard J . Mutations of the PTPN11 gene in therapy-related MDS and AML with rare balanced chromosome translocations. Genes Chromosomes Cancer 2007; 46: 517–521.
Andersen MT, Andersen MK, Christiansen DH, Pedersen-Bjergaard J . Mutations of the NPM1 gene in therapy-related myelodysplasia and acute myeloid leukemia. 2007; submitted for publication.
Pedersen-Bjergaard J, Christiansen DH, Desta F, Andersen MK . Alternative genetic pathways and cooperating genetic abnormalities in the pathogenesis of therapy-related myelodysplasia and acute myeloid leukemia. Leukemia 2006; 20: 1943–1949.
Andersen MK, Christiansen DH, Pedersen-Bjergaard J . Centromeric breakage and highly rearranged chromosome derivatives associated with mutations of TP53 are common in therapy-related MDS and AML after therapy with alkylating agents: an M-FISH study. Genes Chromosomes Cancer 2005; 42: 358–371.
Andersen MK, Christiansen DH, Kirchhoff M, Pedersen-Bjergaard J . Duplication or amplification of chromosome band 11q23, including the unrearranged MLL gene, is a recurrent abnormality in therapy-related MDS and AML, and is closely related to mutation of the TP53 gene and to previous therapy with alkylating agents. Genes Chromosomes Cancer 2001; 31: 33–41.
Andersen MK, Christiansen DH, Pedersen-Bjergaard J . Amplification or duplication of chromosome band 21q22 with multiple copies of the AML1 gene and mutation of the TP53 gene in therapy-related MDS and AML. Leukemia 2005; 19: 197–200.
Sloand EM, Yong AS, Ramkissoon S, Solomou E, Bruno TC, Kim S et al. Granulocyte colony-stimulating factor preferentially stimulates proliferation of monosomy 7 cells bearing the isoform IV receptor. Proc Natl Acad Sci USA 2006; 103: 14483–14488.
Joslin JM, Fernald AA, Tennant TR, Davis EM, Kogan SC, Anastasi J et al. Haploinsufficiency of EGR1, a candidate gene in the del(5q), leads to the development of myeloid disorders. Blood 2007; 110: 719–726.
Liu TX, Becker MW, Jelinek J, Wu WS, Deng M, Mikhalkevich N et al. Chromosome 5q deletion and epigenetic suppression of the gene encoding alpha-catenin (CTNNA1) in myeloid cell transformation. Nat Med 2007; 13: 78–83.
Liu Y, Elf SE, Miyata Y, Sashida G, Deblasio AD, Liu Y et al. Regulation of hematopoietic stem cell quiescence—a novel role for p53. Blood 2007; 110, [abstract 92] 36a.
Le Beau MM, Albain KS, Larson RA, Vardiman JW, Davis EM, Blough RR et al. Clinical and cytogenetic correlations in 63 patients with therapy-related myelodysplastic syndromes and acute nonlymphocytic leukemia: further evidence for characteristic abnormalities of chromosomes no. 5 and 7. J Clin Oncol 1986; 4: 325–345.
Mauritzson N, Albin M, Rylander L, Billstrom R, Ahlgren T, Mikoczy Z et al. Pooled analysis of clinical and cytogenetic features in treatment-related and de novo adult acute myeloid leukemia and myelodysplastic syndromes based on a consecutive series of 761 patients analyzed 1976–1993 and on 5098 unselected cases reported in the literature 1974–2001. Leukemia 2002; 16: 2366–2378.
Pedersen-Bjergaard J, Pedersen M, Roulston D, Philip P . Different genetic pathways in leukemogenesis for patients presenting with therapy-related myelodysplasia and therapy-related acute myeloid leukemia. Blood 1995; 86: 3542–3552.
Smith SM, Le Beau MM, Huo D, Karrison T, Sobecks RM, Anastasi J et al. Clinical-cytogenetic associations in 306 patients with therapy-related myelodysplasia and myeloid leukemia: the University of Chicago series. Blood 2003; 102: 43–52.
Ben Yehuda D, Krichevsky S, Caspi O, Rund D, Polliack A, Abeliovich D et al. Microsatellite instability and p53 mutations in therapy-related leukemia suggest mutator phenotype. Blood 1996; 88: 4296–4303.
Harada H, Harada Y, Tanaka H, Kimura A, Inaba T . Implications of somatic mutations in the AML1 gene in radiation-associated and therapy-related myelodysplastic syndrome/acute myeloid leukemia. Blood 2003; 101: 673–680.
Bacher U, Haferlach T, Schoch C, Kern W, Schnittger S . Implications of NRAS mutations in AML: a study of 2502 patients. Blood 2006; 107: 3847–3853.
Wattel E, Preudhomme C, Hecquet B, Vanrumbeke M, Quesnel B, Dervite I et al. p53 mutations are associated with resistance to chemotherapy and short survival in hematologic malignancies. Blood 1994; 84: 3148–3157.
Padua RA, Guinn BA, Al Sabah AI, Smith M, Taylor C, Pettersson T et al. RAS, FMS and p53 mutations and poor clinical outcome in myelodysplasias: a 10-year follow-up. Leukemia 1998; 12: 887–892.
Niimi H, Harada H, Harada Y, Ding Y, Imagawa J, Inaba T et al. Hyperactivation of the RAS signaling pathway in myelodysplastic syndrome with AML1/RUNX1 point mutations. Leukemia 2006; 20: 635–644.
Preudhomme C, Warot-Loze D, Roumier C, Grardel-Duflos N, Garand R, Lai JL et al. High incidence of biallelic point mutations in the Runt domain of the AML1/PEBP2 alpha B gene in Mo acute myeloid leukemia and in myeloid malignancies with acquired trisomy 21. Blood 2000; 96: 2862–2869.
Harada H, Harada Y, Niimi H, Kyo T, Kimura A, Inaba T . High incidence of somatic mutations in the AML1/RUNX1 gene in myelodysplastic syndrome and low blast percentage myeloid leukemia with myelodysplasia. Blood 2004; 103: 2316–2324.
Steensma DP, Gibbons RJ, Mesa RA, Tefferi A, Higgs DR . Somatic point mutations in RUNX1/CBFA2/AML1 are common in high-risk myelodysplastic syndrome, but not in myelofibrosis with myeloid metaplasia. Eur J Haematol 2005; 74: 47–53.
Chen CY, Lin LI, Tang JL, Ko BS, Tsay W, Chou WC et al. RUNX1 gene mutation in primary myelodysplastic syndrome - the mutation can be detected early at diagnosis or acquired during disease progression and is associated with poor outcome. Br J Haematol 2007; 139: 405–414.
Tartaglia M, Martinelli S, Cazzaniga G, Cordeddu V, Iavarone I, Spinelli M et al. Genetic evidence for lineage-related and differentiation stage-related contribution of somatic PTPN11 mutations to leukemogenesis in childhood acute leukemia. Blood 2004; 104: 307–313.
Bowen DT, Frew ME, Hills R, Gale RE, Wheatley K, Groves MJ et al. RAS mutation in acute myeloid leukemia is associated with distinct cytogenetic subgroups but does not influence outcome in patients younger than 60 years. Blood 2005; 106: 2113–2119.
Bacher U, Haferlach T, Kern W, Haferlach C, Schnittger S . A comparative study of molecular mutations in 381 patients with myelodysplastic syndrome and in 4130 patients with acute myeloid leukemia. Haematologica 2007; 92: 744–752.
Peterson LF, Boyapati A, Ahn EY, Biggs JR, Okumura AJ, Lo MC et al. Acute myeloid leukemia with the 8q22;21q22 translocation: secondary mutational events and alternative t(8;21) transcripts. Blood 2007; 110: 799–805.
Campbell PJ, Green AR . The myeloproliferative disorders. N Engl J Med 2006; 355: 2452–2466.
Christiansen DH, Andersen MK, Pedersen-Bjergaard J . Methylation of p15INK4B is common, is associated with deletion of genes on chromosome arm 7q and predicts a poor prognosis in therapy-related myelodysplasia and acute myeloid leukemia. Leukemia 2003; 17: 1813–1819.
Allen RJ, Smith SD, Moldwin RL, Lu MM, Giordano L, Vignon C et al. Establishment and characterization of a megakaryoblast cell line with amplification of MLL. Leukemia 1998; 12: 1119–1127.
Poppe B, Vandesompele J, Schoch C, Lindvall C, Mrozek K, Bloomfield CD et al. Expression analyses identify MLL as a prominent target of 11q23 amplification and support an etiologic role for MLL gain of function in myeloid malignancies. Blood 2004; 103: 229–235.
Kurokawa M, Tanaka T, Tanaka K, Ogawa S, Mitani K, Yazaki Y et al. Overexpression of the AML1 proto-oncoprotein in NIH3T3 cells leads to neoplastic transformation depending on the DNA-binding and transactivational potencies. Oncogene 1996; 12: 883–892.
Acknowledgements
The study was supported by grants from the Danish Cancer Society. The authors are indebted to Cand. Polit. Severin Olesen Larsen for help in the statistical calculations and to Mr Bent Børgesen for drawing the figures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pedersen-Bjergaard, J., Andersen, M., Andersen, M. et al. Genetics of therapy-related myelodysplasia and acute myeloid leukemia. Leukemia 22, 240–248 (2008). https://doi.org/10.1038/sj.leu.2405078
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.leu.2405078
Keywords
This article is cited by
-
Vemurafenib induces senescence in acute myeloid leukemia and myelodysplastic syndrome by activating the HIPPO signaling pathway: implications for potential targeted therapy
Biology Direct (2024)
-
Combined inhibition of BCL-2 and MCL-1 overcomes BAX deficiency-mediated resistance of TP53-mutant acute myeloid leukemia to individual BH3 mimetics
Blood Cancer Journal (2023)
-
Functional association of NR4A3 downregulation with impaired differentiation in myeloid leukemogenesis
Annals of Hematology (2022)
-
Characteristics and outcomes of patients with therapy-related acute myeloid leukemia with normal karyotype
Blood Cancer Journal (2020)
-
Genetic Pathway in the Pathogenesis of Therapy-Related Myeloid Neoplasms: A Literature Review
Oncology and Therapy (2020)