Abstract
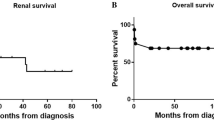
Anti-neutrophil cytoplasmic antibody (ANCA)-associated systemic vasculitis is reported mainly in adults. Studies in children are limited. The current study retrospectively analyzed the clinical characteristics and pathology of ANCA-associated systemic vasculitis in children in our hospital during the past 7 years. Twenty-four pediatric patients were diagnosed as having ANCA-associated systemic vasculitis, including 19 patients with microscopic polyangiitis (MPA), one with Wegener’s granulomatosis (WG), three with propylthiouracil (PTU)-induced ANCA-positive vasculitis and one with anti-glomerular basement membrane (GBM) disease. Of patients with primary ANCA-associated systemic vasculitis (MPA and WG), with an average age of 10.8±2.8 (6–14) years, 18 patients (90%) were female and two (10%) were male. Nineteen patients (95%) were p-ANCA/MPO-ANCA positive and one (5%) was c-ANCA/PR3-ANCA positive. The interval between onset and diagnosis was 8.5±24.3 (0.2–108) months. The majority of the patients (85%) had multi-organ involvement. All patients had clinical evidence of renal involvement and presented with hematuria and proteinuria. Of 20 patients, 16 (80%) also had acute renal failure, and five patients were dialysis dependent. Nine patients underwent renal biopsy and were diagnosed with necrotizing and crescentic glomerulonephritis. However, six biopsies showed immune complex deposition. All patients received immunosuppressive therapy including prednisone and cyclophosphamide, and ten patients also received intravenous administration of methylprednisone pulse therapy according to their clinical situation and renal pathology. Sixteen patients achieved clinical remission, and four patients presented as treatment failure. Patients were followed up for 12.3±5.1 months (median 12 months; range 1 to 91 months). Ten patients maintained their clinical remission, and ten progressed to renal failure requiring dialysis. Our study showed that the clinical features and pathology of primary ANCA-associated systemic vasculitis in children were similar to those of adults, but there were a predominance of female patients and late diagnoses. We suggest that early recognition and prompt aggressive treatment might improve outcome.


Similar content being viewed by others
References
Jennette JC, Falk RJ, Andrassy K, Bacon PA, Churg J, Gross WL, Hagen EC, Hoffman GS, Hunder GG, Kallenberg CG (1994) Nomenclature of systemic vasculitides: proposal of an international consensus conference. Arthritis Rheum 37:187–192
Luqmani RA, Bacon PA, Moots RJ, Janssen BA, Pall A, Emery P, Savage C, Adu D (1994) Birmingham Vasculitis Activity Score (BVAS) in systemic necrotizing vasculitis. QJM 87:671–678
Xin G, Zhao MH, Wang HY (2004) Detection rate and antigenic specificities of antineutrophil cytoplasmic antibodies in Chinese patients with clinically suspected vasculitis. Clin Diagn Lab Immunol 11:559–562
Wyatt RJ, Emancipator SN, Kon V, Waldo FB, Donadio J, Grande JP, Andreoli SP, Glassock RJ (1997) IgA nephropathy databank: development of a system for management of renal biopsy acquired data. Am J Kidney Dis 29:817–828
Nachman PH, Hogan SL, Jennette JC, Falk RJ (1996) Treatment response and relapse in ANCA-associated MPA and glomerulonephritis. J Am Soc Nephrol 7:33–39
Ozen S (2005) Problems in classifying vasculitis in children. Pediatr Nephrol 20:1214–1218
Walters MD, Savage CO, Dillon MJ, Lockwood CM, Barratt TM (1988) Antineutrophil cytoplasm antibody in crescentic glomerulonephritis. Arch Dis Child 63:814–817
Erdogan O, Oner A, Demircin G, Bulbul M, Memis L, Uner C, Kiper N (2004) A boy with consecutive development of SLE and Wegener granulomatosis. Pediatr Nephrol 19:438–441
Hijosa MM, Roman LE, Camblor CF, Garcia ML, Salcedo DP, Torres MN (2005) Anti-GBM and anti-MPO antibodies coexist in a case of pulmonary renal syndrome. Pediatr Nephrol 20:807–810
Wang Y, Zhao MH, Yu J, Xin G, Liu YC, Zhang YK, Wang HY (2004) The clinical and pathological characteristics of Chinese elderly patients with anti-neutrophil cytoplasmic autoantibodies associated small vessel vasculitis. Exp Gerontol 39:1401–1405
Ellis EN, Wood EG, Berry P (1995) Spectrum of disease associated with anti-neutrophil cytoplasmic autoantibodies in pediatric patients. J Pediatr 126:40–43
Hattori M, Kurayama H, Koitabashi Y (2001) Antineutrophil cytoplasmic autoantibody-associated glomerulonephritis in children. J Am Soc Nephro 12:1493–1500
Hogan SL, Nachman PH, Wilkman AS, Jennette JC, Falk RJ (1996) Prognostic markers in patients with antineutrophil cytoplasmic autoantibody-associated microscopic polyangiitis and glomerulonephritis. J Am Soc Nephrol 7:23–32
Haas M, Eustace JA (2004) Immune complex deposits in ANCA-associated crescentic glomerulonephritis: a study of 126 cases. Kidney Int 65:2145–2152
Beimler JH, Andrassy K (2004) Cyclophosphamide treatment in systemic necrotizing vasculitis and lupus nephritis. How long? How much? Pediatr Nephrol 19:949–955
Valentini RP, Smoyer WE, Sedman AB, Kershaw DB, Gregory MJ, Bunchman TE (1998) Outcome of antineutrophil cytoplasmic autoantibodies-positive glomerulonephritis and vasculitis in children: a single-center experience. J Pediatr 132:325–328
Besbas N, Ozen S, Saatci U, Topaloglu R, Tinaztepe K, Bakkaloglu A (2000) Renal involvement in polyarteritis nodosa: evaluation of 26 Turkish children. Pediatr Nephrol 14:325–327
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yu, F., Huang, JP., Zou, WZ. et al. The clinical features of anti-neutrophil cytoplasmic antibody-associated systemic vasculitis in Chinese children. Pediatr Nephrol 21, 497–502 (2006). https://doi.org/10.1007/s00467-006-0028-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-006-0028-3