Abstract
Major cutaneous vascular complications of systemic sclerosis (SSc) are secondary Raynaud’s phenomenon (RP) and digital ulcers. Even though SSc is a rare disease, timely and appropriate management of its vascular complications is mandatory for reducing the rate of major impairment. It should therefore be aware to physicians from different specialties. We evaluated the diagnostic and therapeutic approach toward secondary RP and ulceration in SSc patients at 28 German clinical centers at the time of initiation of the German network for Systemic Scleroderma (DNSS). We retrieved data via questionnaires and from the DNSS patient registry. Management of RP and ulcerations in SSc were heterogeneous at initiation of the network, reflecting a sometimes insufficient use of the diagnostic and therapeutic possibilities. As such, (1) calcium channel blockers were the first line therapy in most centers; but often in insufficient dosages, and (2) only 21.2% of patients with acral ulceration had received prostacyclins when recruited into the network. The sometimes insufficient care of vascular complications of SSc in Germany revealed the need for their standardized management, e.g. within a network for SSc and for consensus on a diagnostic or therapeutic algorithm.
Similar content being viewed by others
Introduction
Major cutaneous vascular complications of systemic sclerosis (SSc) are Raynaud’s phenomenon (RP) and digital ulcers.
RP is characterized by recurrent spasms of small digital arterioles and arteries mostly of fingers, usually triggered by cold and emotional stress. Clinically it is characterized by a sudden pallor of individual digits which is followed by reactive hyperaemia, in severe cases also by cyanosis.
In SSc, RP is the major presenting symptom in more than 90% of patients [1]. It is also frequently encountered in other autoimmune diseases such as SLE (in 10–45% of patients), Sjögren syndrome (ca. 30%), dermatomyositis (ca. 20%), rheumatoid arthritis (10–20%) [2]. Though less frequent than primary RP, secondary RP has a more severe course and in SSc it is frequently associated with development of digital necrosis, ulcers or even gangrene. According to the vascular hypothesis developed by Le Roy, RP is also part of the initial events in the pathogenesis of SSc, serving as a trigger for the fibrotic processes [1, 3]. RP-like events are also observed in other involved organs (i.e. the heart) where they are followed by fibrotic disease manifestations [1, 3].
For these reasons a timely and appropriate diagnosis and therapy of RP are of utmost importance. Also, in light of the high prevalence of primary RP (13–20% in northern France, and 8–10% in Massachusetts, USA) [2, 4], appropriate diagnostic measures to recognize and differentiate primary from secondary RP would provide re-assurance to many patients with primary RP [2]. However, SSc is a rare disease, and patients with vascular complications due to SSc present to physicians from different specialties such as dermatology or rheumatology. So it may not be guaranteed, that management of SSc will have the same quality throughout. We therefore wondered what the status would be for the diagnostic and therapeutic approach toward RP and digital ulcerations in SSc patients around Germany.
This question was addressed in context with the initiation of the German Network for Systemic Scleroderma (DNSS) in 2003. The Network was established in order to improve clinical care of the various symptoms and complications of SSc. It encompasses rheumatologists, dermatologists, pulmonologists and nephrologists, who built up a nation-wide patient registry to fulfil the prerequisites for an analysis of diagnostic and therapeutic measures in a sufficiently high number of patients.
In this study the registry of the DNSS and additional questionnaires were used to investigate the status of diagnostic and therapeutic procedures applied in patients with cutaneous vascular complications when the network was established. We found that the management of RP was rather heterogeneous at initiation of the network.
There was no generally approved diagnostic approach nor did all centers use the full range of therapeutic modalities. As such, some centers did not use the full dosage for, e.g. calcium channel blockers, while others were reluctant in applying iloprost for ulcerations or in considering use of sildenafil or bosentan.
Our results reveal that the status of diagnosis and especially treatment of vascular complications in patients with SSc needed to be improved. By establishing a network of clinical centers specialized in SSc both development of standardized care and, correspondingly, using these standards on the majority of patients with SSc in Germany could be attained.
Methods
Questionnaire to participating centers
For this study we performed a survey by questionnaires at the 28 initially participating German medical centers at the induction of the DNSS, i.e. at Aachen, Bad Bramstedt, Bad Nauheim, Berlin, Bonn, Dresden, Duesseldorf, Frankfurt, Freiburg, Giessen, Goettingen, Hamburg, Hanover, Kaiserslautern, Cologne, Leipzig, Luebeck, Mainz, Munich, Muenster, Regensburg, Tuebingen, Ulm, Witten, and Wuerzburg). These centers were experienced in management of patients with SSc, and the questionnaire focused on the diagnostic and therapeutic procedures by which these centers approached patients with RP in Germany.
The questionnaire contained detailed questions on:
-
1.
Diagnostic procedures, such as the use of:
-
Standardized questionnaire to obtain information about RP and possibly associated diseases
-
Standardized documentation of the course of disease (e.g. diaries for patients to record frequency and severity of attacks)
-
Standardized documentation of the formation, the presence and the course of vascular complications
-
Diagnostic means such as acral oscillography, capillary microscopy, duplex or Doppler sonography, angiologic MRT, digital subtraction angiography
-
-
2.
Therapeutic procedures and regimens (first, second and third line):
-
Physiotherapy
-
Recommendation for heatable devices
-
Use of vasoactive medication, such as calcium channel blockers, ACE inhibitors, AT II blockers, iloprost, sildenafil, or bosentan
-
Use of rheological drugs
-
Maximum dosages
-
-
3.
Documentation of therapy efficacy by:
-
Standardized questionnaires
-
Diagnostic procedures
-
(Table 1 contains a translation of the questionnaire)
The German Network for Systemic Scleroderma (Deutsches Netzwerk für Systemische Sklerodermie—DNSS)
The DNSS was founded in October 2003 supported by a grant from the German Ministry of Education and Research (BMBF). The Network comprises different subspecialties, i.e. rheumatologists, dermatologists, pulmonologists and nephrologists.
The Ethics Committee of the coordinating center, i.e. the Cologne University Hospital, gave a positive vote on the patient information and consent form for the registry. On the basis of this document, all participating centers sought the approval of their local ethics committees prior to registering patients.
By August 2007, more than 1,881 patients had been registered.
Data recording of DNSS patients
The DNSS maintains a centralized online patient registry in which all patient data from the four-page DNSS-patient registration form are entered. The online patient registry is using the MACRO software for Clinical Trials. A Central Office for Coordination of the DNSS validates the registration forms before they are finally entered into the online registry.
Patient data are recorded at the time of entry to the DNSS and annually thereafter. For this study we retrieved and evaluated data from patients at the time of entry in the DNSS.
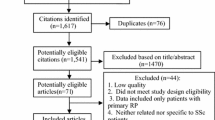
Statistical analyses
The data from the questionnaire and from the patient registry were statistically analyzed using Excel and SPSS 15.0 for tabular and graphic representation. Statistical evaluation was performed using contingency table tests (χ2-test) to describe significant differences or associations. When multiple tests were performed, only P values below 0.05 are mentioned. In the questionnaire the percentage of missing data was never above 5%. In the DNSS registry no accurate data about therapy from 1,881 patients were given in less than 15%, leaving complete evaluable data sets of 1,616 patients.
Results
At the beginning of the project, we performed a survey by questionnaires in 28 German medical centers participating in the DNSS in order to evaluate the status of diagnostic and therapeutic procedures in patients with cutaneous vascular complications of SSc. The focus of the survey was on RP as it is the major presenting symptom of SSc.
Diagnostic procedures
At initiation of the DNSS the centers estimated that during 1 year they on average attended approximately 30 patients with primary and 65 patients with secondary RP. The predominance of secondary RP (which usually comprises <10%) is due to the selection of centers which treat patients with SSc.
Follow-up visits of patients were scheduled every 5.6 months on average when an underlying autoimmune disease had been diagnosed (secondary RP); patient with RP were examined every 11.4 months or when repeated visits were thought to be necessary.
Our survey showed that prior to the induction of the network none of the participating centers used a standardized questionnaire to obtain information about RP when interviewing their patients on their first visit. Consequently, they did not use standardized check lists about possibly underlying causes to distinguish between primary and secondary RP. History of the patient and findings of the physical exam were instead documented on routine charts as used for most other patients. Three centers distributed diaries to patients requesting the documentation of frequency and severity of attacks.
Relevant accompanying conditions or complications associated with secondary RP in SSC are atrophy of skin over fingers and thinning of digits, digital pits and acral ulcerations. Documentation of the formation, the presence and the course of these complications is useful for appropriate management. The presence of RP and of its complications was recorded regularly on patient charts. Details of these complications (such as beginning, exact localization and extent of digital ulcerations) were documented in 16 centers (57.1%). In 13 centers these findings were also documented photographically.
Acral oscillography in addition with a standardized provocation test (cooling down to 10°C) is considered do be one important diagnostic procedure to confirm the diagnosis of RP. An acral oscillography was regularly ordered at 11 centers, while it would have been accessible in 15 centers.
For the ensuing distinction between primary and secondary RP capillary microscopy is an appropriate diagnostic tool as it helps to detect characteristic structural alteration of vessels. Capillary microscopy also was not used routinely and regularly in all centers: only 16 of the institutions performed an analysis with capillary microscopy, while the facilities would have been present in 19 centers.
Alternative diagnostic procedures such as thermography or laser Doppler velocity meter were only used at five centers.
Almost all (23) centers, however, regularly had antinuclear antibodies determined when they suspected an associated autoimmune disease, i.e. a secondary RP.
As SSc was described to be associated with a higher percentage of other anomalies in peripheral vessels in the extremities, an investigation of the larger vessel was considered in half of all centers. Only seven utilized duplex or Doppler sonography instead of mere physical exam. Interestingly, more expensive and advanced techniques such as digital subtractive angiography or even angiologic MRT were also used in single cases for revealing anomalies of vascular status and diagnosing RP.
Therapeutic regimens
Concerning the therapeutic approach to RP, only six of the DNSS centers pursued a fixed therapeutic algorithm. All centers stated that they did not make their therapeutic procedure dependent on presence of primary or secondary RP, but rather on the success or failure of their preferred first line treatments.
The efficacy or outcome of therapy was evaluated in a standardized way by questionnaires in 18 centers, or by diaries in only one center or by questionnaire and diary in two centers. Also ten centers used repeated analysis by acral oscillography as another means to evaluate possible improvement of RP.
Physiotherapy, encompassing, e.g. paraffin kneading, paraffin baths, and/or lymph drainage, was encouraged by 22 centers.
The use of calcium channel blockers, especially nifedipine, diltiazem and amlodipine, was the first line therapy in most (24) centers. Yet, no all centers tried to regularly strive for dosages considered to be high enough to treat (secondary) RP [5, 6]; as such 23 centers denied to aim at 360 mg for diltiazem or for at least 10 mg amlodipine, and 20 centers did not regularly attempt to give at least 40 mg for nifedipine.
ACE inhibitors and AT II blockers were not a medication of first choice at 14 and 19 centers, respectively.
Administration of the vasodilator iloprost (usually given in the recommended dosage of 0.5 g–2 μg/kg b.w. and over five or more days) was considered in almost all centers (23 of 25), but it was not given very regularly for severe RP or ulceration. In 15 centers it was only exclusively (but not regularly) applied when digital ulcerations were present, in six centers when other vasodilators had not been efficacious. Reasons given for reluctant use of iloprost were high costs, the need for hospital referral or the lack of approval of this drug for RP in Germany (off-label use).
Regarding the subspecialties, all departments of internal medicine [15] and eight out of ten dermatological departments had administered iloprost at least once, while two dermatological departments had not given iloprost, independent from occurrence from ulcers.
Alternative drugs for treatment or prophylaxis severe RP and digital ulcerations against ulcers or for prevention of ulcers are sildenafil and bosentan. Twenty centers never used sildenafil and 17 centers never used bosentan, neither for ulceration nor for severe and recalcitrant RP. Only rheumatological centers had administered bosentan and sildenafil at the initiation of the network.
Patient data at entry into the DNSS
We then analysed the status of patient care when they were first recruited and registered at the DNSS. These patients had either been managed already previously by the centers or by referring physicians, such as general practitioners, dermatologists or specialists in internal medicine.
Twenty-two centers encouraged physiotherapy. It was actually performed by 53% of patients with RP, and by 56% of all patients with ulcers within the DNSS.
In the DNSS 408 patients (24.1%) had acral ulcerations. According to the data retrieved from the DNSS registry about 60% of patients with RP (without ulcers) and 40% of the patients with acral ulcerations did not receive a vasoactive medication when they were first presented to the centers of the DNSS (P < 0.0005).
Among the treated patients calcium channel blockers were administered in one third of all cases (three times as often as prostacyclins). Even in 27.8% of patients who already suffered from digital ulcerations at the time of initial registration in the DNSS centers calcium channel blockers was the exclusive therapy.
ACE inhibitors were prescribed to 20.5% of patients with Raynaud (in 49% in combination with another vasodilator) and even still to 24.2% with ulcers (in 55% in combination with a vasodilator) (P = 0.12).
Topical nitrates were prescribed to 1.8% of patients with RP and 2.6% of patients with ulcers. Alpha receptor blockers and AT II blocker were taken by less than 2.5% of the patients.
The main indication for use of iloprost was the presence of acral ulceration according to the questionnaire. However, only 21.2% of patients with acral ulceration actually received prostacyclins (in 10.7% in combination with another vasodilator) prior to their recruitment into the DNSS.
Among the only infrequently used vasoactive drugs bosentan (5.5%) and sildenafil (3.4%), only bosentan was prescribed significantly more often to patients with ulcers compared to patients with uncomplicated secondary RP (P = 0.0036; P = 0.071).
Aspirin for pro-rheological purposes was administered to 11% of patients with or without RP and significantly more frequently to patients with ulcers (14%)
(P = 0.015). Pentoxifyllin was used by 8% of patients with RP and by 6% with ulcers.
Discussion
We analyzed the status of diagnostic and therapeutic procedures in patients with cutaneous vascular complications of SSc at the initiation of the network. The focus of the survey was on RP and digital ulcerations.
We found that at the time of initiation of the German Network for Systemic Scleroderma (Deutsches Netzwerk für Systemische Sklerodermie—DNSS), the diagnostic and therapeutic approach toward primary and secondary RP were rather heterogeneous among the 28 participating German medical centers. There was no generally approved diagnostic algorithm among centers specialized in treating patients with SSc, nor did all centers apply the full range of therapeutic modalities. As such, they had not always exploited the full dosage for the standard therapies such as calcium channel blockers, or they were reluctant with off label use of, e.g. sildenafil and especially iloprost.
When analysing patient data from the central registry of the DNSS we revealed that, correspondingly, the status of management of vascular complications in patients was insufficient in several cases at the time of first registration at the DNSS.
Diagnostic procedures
One major reason for the heterogeneous diagnostic approaches apparently was a lack of consensus on diagnostic algorithm. Limited availability of certain diagnostic procedures in some centers was only a minor reason as acral oscillography and capillary microscopy would have been accessible in more centers (acral oscillography in 15 and capillary microscopy in 19) than those that regularly performed them (11 and 16 centers, respectively).
Although primary RP is markedly more frequent than secondary RP and only rarely results in severe complications such as acral ulcers [2], the relevance and possible sequela of secondary RP warrant the necessary efforts to confirm diagnosis of RP and to distinguish secondary from primary RP. Since attacks of secondary RP in SSc are considered to be one of the triggers for the ensuing fibrotic processes its early detection and ensuing treatment may even provide a chance to retard sclerosis [1, 7].
Lack of consensus on diagnostic procedures often results from lack of agreement on the diagnostic or predictive value of those procedures. There are only few studies on the predictive value of acral oscillography or plethysmography for recognizing the presence of (primary and secondary) RP [8], but at least there appears to be a rationale and good experience for its use with a standardized provocation tests (cooling down to 10°C), partly because vasospastic diathesis can be detected before clinical signs of RP become apparent [9].
For distinguishing between primary and secondary RP in the context of autoimmune collagen-vascular diseases such as SSc, the association of secondary RP with morphological, structural alterations of vessels can well be exploited by capillary microscopy or nailfold capillaroscopy, a non-invasive and safe technique. Although altered vessel architecture has also been observed in primary RP [10], enlarged vessels and avascular areas present a predictive value of approximately 47% for development of SSc [11].
There was wide acceptance among the centers to use determination of antinuclear antibodies as a means to detect a possibly underlying autoimmune disease in case of RP and to thus diagnose a secondary RP. The presence of high titres of antinuclear antibodies in patients with RP is indeed a useful predictor for development of autoimmune, collagen-vascular disease, having a predictive value of approximately 50% [2, 12].
There are not sufficient data yet on the predictive or diagnostic value of alternative diagnostic procedures such as thermography or laser Doppler velocity meter. A thorough evaluation should also analyse general applicability in a high number or centers.
Obviously, practicability and costs were two other criteria in the decision making to find diagnostic procedures. We had not explicitly included these parameters in our questionnaire, but it was mentioned in the commentaries, that those diagnostic procedures would be preferred which are easy to perform and not expensive.
A standardization of diagnostic protocol is required to raise valid data on the prognostic relevance of the patient’s individual vascular status, for early diagnosis of SSc and for clinical studies. As pointed out in a recent review, standardization in evaluating secondary RP is a crucial point not generally reached yet [13].
One aim of the DNSS was to develop recommendations for the diagnosis of the various symptoms and complications of SSc (Hunzelmann et al. submitted). Within the DNSS we now agreed that capillary microscopy and determination of antinuclear antibodies present appropriate diagnostic procedures to distinguish primary from secondary RP and that acral oscillography should be used to confirm diagnosis of RP; in its absence we find it helpful to show photographs of true RP to patients in order to confirm diagnosis and differentiate from, e.g. cold-induced pallor. We also recommend the use of standardized questionnaires in order not to overlook valuable information on, e.g. possible causes for secondary RP or time of onset of RP (if it is long, it increase the likelihood of the limited SSc instead of diffuse SSc [14] (Hunzelmann et al. manuscript submitted, Sunderkötter et al. manuscript in preparation). Patients should use diaries in which they document frequency, duration and severity (e.g. by semi quantitative scale for pain frequency and duration) of attacks of RP. This has been a reliable parameter also to evaluate efficacy of therapies [15]. Relevant accompanying conditions or complications associated with secondary RP in SSc are atrophy of skin over fingers and thinning of digits, digital pits and digital ulcerations. These conditions demand different therapeutic procedures (see below) [6, 13, 16]. Therefore documentation of these complications is relevant and is now encouraged for all centers within the network.
As SSc was described to be associated with a higher percentage of other anomalies in peripheral vessels in the extremities [17, 18], an investigation of the larger vessel was considered in half of all centers. On basis of applicability and costs this could best be done via duplex or Doppler sonography, while more expensive and advanced techniques such as digital subtractive angiography or even angiologic MRT may entail higher risks to the patient and higher costs.
Our data suggest that a general screening with easy applicable techniques such as duplex or Doppler sonography had not been performed by the centers forming the DNSS.
Therapy
Our questionnaire had revealed that at initiation of the DNSS not all centers exploited the full range of therapeutic modalities, i.e. they have not always used the full dosage range for the standard therapies such as calcium channel blockers, or they were reluctant in applying off-label use of, e.g. sildenafil.
These results from the questionnaire were consistent with data obtained from the patient registry of the DNSS as on recruitment of these patients therapies of their RP did not appear to be completely appropriate. It was remarkable—and needs to be improved—that about 60% of patients with RP (without ulcers) and 40% of the patients with digital ulcerations did not receive a vasoactive medication when they were first referred to the centers of the DNSS. It should be mentioned that these data reflect the therapeutic approaches of both the centers and of the referring physicians. Among the latter were general practitioners, dermatologists or specialists in internal medicine/rheumatology. In addition, the data were obtained before therapeutic guidelines had been recommended within the DNSS (August 2007).
The predominance of calcium channel blockers as therapy of first choice in RP reflects evidence based data [5]. Yet, the full dosage considered to be necessary for full efficacy was not always thrived for—independent from adverse side effects.
The rather infrequent use of iloprost among patients (only 21% of patients with acral ulceration actually received prostacyclins) at the time of registry was noteworthy. In the questionnaire almost all centers (23 of 25) had stated that they would administrate iloprost. Yet, 15 centers at the initiation of the network had restricted its use to patients with acral ulcerations. This apparently is one reason for low prevalence of iloprost treatment in SSc patients with digital ulcerations. Also it needs to be considered that iloprost is not approved for these indications in Germany. Correspondingly, lack of approval as well as high costs and need for hospital referral were indeed given as reasons for not using it in higher frequency.
Since there is sufficient evidence for its efficacy in secondary RP and in digital ulcerations [19] a more frequent use of this drug is warranted.
It is also noteworthy that in over 20% ACE inhibitors were administered to patients with RP, but though we asked specifically for treatment of RP, we cannot exclude that in some of these cases ACE inhibitors were given for other indication such as hypertension
Reasons for the sometimes suboptimal therapeutic approaches clearly appears to be the lack of guidelines on diagnostic and therapeutic management of primary and secondary RP, and the absence of good, evidence-based, general reviews on the treatment of RP at the time when the data were obtained. In the meantime such reviews have been published [13, 20, 21] (partly because of the results of this survey [20, 21]), complementing other excellent reviews or Cochrane analyses [5, 19, 22]. These sources have become the basis for a consensus on diagnostic and therapeutic algorithm within the DNSS [20].
As mentioned above, attacks of secondary RP are considered as one of the triggers for the ensuing fibrotic processes. So, adequate use of all therapeutic options would be even more important, not only to relieve discomfort of RP, but also to detect scleroderma vascular disease at an early stage, and not to miss the chance to retard sclerosis.
In summary, our analysis revealed that the status of diagnosis and treatment of vascular complications in patients with SSc needed to be improved. It therefore underlined the necessity for foundation of a coordinated network of clinical centers in order to discuss, develop and establish recommendations for the diagnosis as well as the treatment of cutaneous vascular complications in SSc.
Such recommendations should prevent that patients with SSc present with digital ulcers without having been treated with at least iloprost or sildenafil.
References
LeRoy EC (1996) Systemic sclerosis. A vascular perspective. Rheum Dis Clin North Am 22(4):675–694
Block JA, Sequeira W (2001) Raynaud’s phenomenon. Lancet 357(9273):2042–2048
LeRoy EC (1989) The pathogenesis of systemic sclerosis. Clin Exp Rheumatol 7(Suppl 3):S135–S137
Fraenkel L, Zhang Y, Chaisson CE, Maricq HR, Evans SR, Brand F et al (1999) Different factors influencing the expression of Raynaud’s phenomenon in men and women. Arthritis Rheum 42(2):306–310
Thompson AE, Shea B, Welch V, Fenlon D, Pope JE (2001) Calcium-channel blockers for Raynaud’s phenomenon in systemic sclerosis. Arthritis Rheum 44(8):1841-1847
Riemekasten G, Sunderkötter C (2006) Vasoactive therapies in systemic sclerosis. Rheumatology (Oxford) 45(Suppl 3):iii49–iii51
Sunderkötter C, Riemekasten G (2006) Pathophysiology and clinical consequences of Raynaud’s phenomenon related to systemic sclerosis. Rheumatology (Oxford) 45(Suppl 3):iii33–iii35
Planchon B, de Faucal P, Essboui S, Grolleau JY (1986) A quantitative test for measuring reactivity to cold by the digital plethysmograph technique: application to 66 control subjects and 65 patients with Raynaud’s phenomenon. Angiology 37(6):433–439
Pistorius MA, Planchon B, de Faucal P (1994) Plethysmographic cold test for diagnosis and evaluation of the severity of Raynaud’s phenomenon. Validation of the method by factorial analysis of correspondences in 541 patients. Int Angiol 13(1):10–14
Bukhari M, Herrick AL, Moore T, Manning J, Jayson MI (1996) Increased nailfold capillary dimensions in primary Raynaud’s phenomenon, systemic sclerosis. Br J Rheumatol 35(11):1127–1131
Spencer-Green G (1998) Outcomes in primary Raynaud phenomenon: a meta-analysis of the frequency, rates, and predictors of transition to secondary diseases. Arch Intern Med 158(6):595–600
Sarkozi J, Bookman AA, Lee P, Keystone EC, Fritzler MJ (1987) Significance of anticentromere antibody in idiopathic Raynaud’s syndrome. Am J Med 83(5):893–398
Hummers LK, Wigley FM (2003) Management of Raynaud’s phenomenon and digital ischemic lesions in scleroderma. Rheum Dis Clin North Am 29(2):293–313
Walker UA, Tyndall A, Czirjak L, Denton C, Farge-Bancel D, Kowal-Bielecka O et al (2007) Clinical risk assessment of organ manifestations in systemic sclerosis: a report from the EULAR scleroderma trials and research group database. Ann Rheum Dis 66(6):754–763
Merkel PA, Herln K, Martin RW, Anderson JJ, Mayes MD, Bell P et al (2002) Measuring disease activity and functional status in patients with scleroderma and Raynaud’s phenomenon. Arthritis Rheum 46(9):2410–2420
Wigley FM, Seibold JR, Wise RA, McCloskey DA, Dole WP (1992) Intravenous iloprost treatment of Raynaud’s phenomenon and ischemic ulcers secondary to systemic sclerosis. J Rheumatol 19(9):1407–1414
Veale DJ, Collidge TA, Belch JJ (1995) Increased prevalence of symptomatic macrovascular disease in systemic sclerosis. Ann Rheum Dis 54(10):853–855
Taylor MH, McFadden JA, Bolster MB, Silver RM (2002) Ulnar artery involvement in systemic sclerosis (scleroderma). J Rheumatol 29(1):102–106
Pope J, Fenlon D, Thompson A, Shea B, Furst D, Wells G et al (2000) Iloprost and cisaprost for Raynaud’s phenomenon in progressive systemic sclerosis. Cochrane Database Syst Rev 2:CD000953
Sunderkötter C, Riemekasten G (2006) Raynaud phänomen in der Dermatologie: Teil 2: Therapie. Hautarzt 57:927–938
Distler M, Distler J, Ciurea A, Kyburz D, Muller-Ladner U, Reich K et al (2006) Evidence-based therapy of Raynaud’s syndrome. Z Rheumatol 65(4):285–289
Pope J, Fenlon D, Thompson A, Shea B, Furst D, Wells G et al (2000) Ketanserin for Raynaud’s phenomenon in progressive systemic sclerosis. Cochrane Database Syst Rev 2:CD000954
Acknowledgments
This work was supported by grants from BMBF Fkz 01 GM 0310 (C. S., I. H. and G. R.).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Herrgott, I., Riemekasten, G., Hunzelmann, N. et al. Management of cutaneous vascular complications in systemic scleroderma: experience from the German network. Rheumatol Int 28, 1023–1029 (2008). https://doi.org/10.1007/s00296-008-0556-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-008-0556-1